Authors
Dr Rael Mutai, Liverpool School of Tropical Medicine Kenya
Professor Charles Ameh, Liverpool School of Tropical Medicine
UNAIDS data show that today, 29.8 million of the 39 million people living with HIV globally are receiving life-saving treatment. Around the world, 9.2 million people living with HIV do not have access to lifesaving antiretroviral therapy. Every minute, a life is lost to AIDS. Access to antiretroviral therapy has expanded massively in sub-Saharan Africa and Asia and the Pacific, which together are home to about 82% of all people living with HIV.
In eastern Africa, steady increases in the availability of HIV resources have enabled countries to expand their HIV responses massively over the past two decades. Achieving the 2025 global HIV testing and treatment targets of 95% of the people who are living with HIV knowing their HIV status, 95% of the people who know that they are living with HIV being on lifesaving antiretroviral treatment, and 95% of people who are on treatment being virally suppressed (95-95-95), require maintaining high level of resource commitment while significantly increasing both the effectiveness and efficiency of programmes.
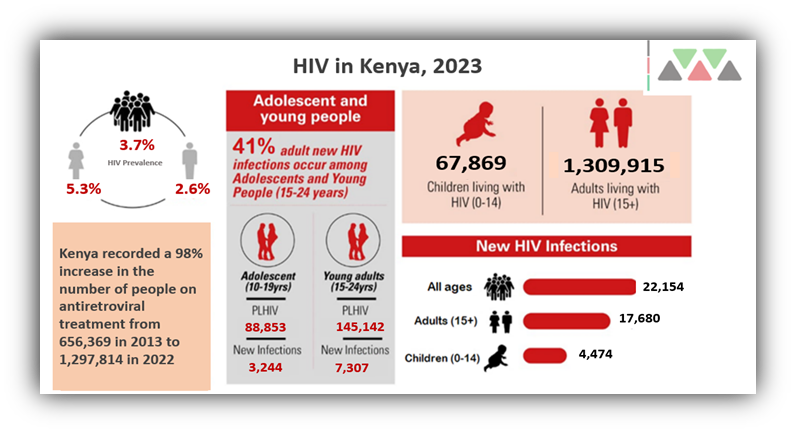
In many high HIV burden countries, HIV/AIDS prevalence is high among women of reproductive age and is an important contributing factor to high maternal morbidity and mortality. The Kenya HIV Prevalence and Mother to Child Transmission of HIV (MTCT) rates have declined significantly to 3.7% and 8.6% respectively (NACC 2023). Adult HIV prevalence in Tanzania is estimated at 5 percent, with regional HIV prevalence ranging from 0.5 percent (Zanzibar) to 11.4 percent (Njombe). HIV is a generalized epidemic in Tanzania but there are also concentrated sub-epidemics among key populations. Women and girls continue to be disproportionately affected compared to men, with adolescent girls and young women accounting for 80 percent of all new HIV infections.
HIV and AIDS influences the risk of maternal death through a variety of mechanisms. Pregnancy and HIV and AIDS both increase women’s susceptibility to acquiring malaria and to developing active tuberculosis, which are associated with increased risk of maternal death.
While progress has been made towards increasing HIV-testing during pregnancy and providing antiretroviral therapy (ART) to prevent vertical mother-to-child transmission, insufficient integration of HIV services into reproductive, maternal, newborn, child and adolescent health (RMNCAH) care is a major challenge. For many women around the world, antenatal care is their first adult contact with the health care system, representing an important opportunity to screen for, prevent and treat chronic diseases such as HIV and AIDS; however, many women who test positive for HIV during pregnancy do not receive the follow-up care that they need.
Documented barriers to women beginning and continuing HIV treatment include broader health system issues such as poor quality of care and social determinants including geographic and economic barriers that are also associated with poor uptake and retention. All women should know their HIV status and understand the importance of HIV prevention. knowledge of HIV status, through HIV testing and counselling, is especially important during pregnancy, childbirth, and breastfeeding, since women with HIV can transmit the virus to their infants during these times.
With funding from the Global Fund, the Liverpool School of Tropical Medicine in collaboration with the Ministries of Health and other partners in Kenya and Tanzania, has implemented a programme (2021-2023) that aims to improve the availability and quality of integrated HIV, TB and Malaria services provided at healthcare facilities as part of antenatal and postnatal care (ANC and PNC). The programme builds the competencies of primary healthcare facilities and frontline healthcare workers on quality integrated service delivery for improved maternal and newborn health outcomes.
In the last decade, both Kenya and Tanzania brought treatment to scale, new infections and AIDS-related deaths have declined, but the progress is not enough. We must redouble our efforts. The journey to end AIDS as a public health threat by 2030 is getting tighter.
The 2023 World Aids report titled LET COMMUNITIES LEAD is not only a celebration of the critical role of communities including community health systems on ending the HIV/AIDS scourge. It is a call to action to decision-makers to fully support the life-saving work of communities and to clear away the barriers that stand in their way.