Authors
Martin Eyinda, Technical Officer – Liverpool School of Tropical Medicine (LSTM) Kenya
Duncan Shikuku, Senior Technical Officer - Liverpool School of Tropical Medicine (LSTM) Kenya
Irene Nyaoke, Senior Technical Officer - Liverpool School of Tropical Medicine (LSTM) Kenya
Rael Mutai, Regional Technical Advisor- Liverpool School of Tropical Medicine (LSTM) Kenya
Lucy Nyaga, Country Director-Liverpool School of Tropical Medicine (LSTM) Kenya
Charles Ameh, Professor Global Health, Head Emergency Obstetric and Quality of Care Unit, Liverpool School of Tropical Medicine (LSTM) United Kingdom
Background
There is slow progress in reduction of global maternal mortality. About 27 percent of global maternal deaths are due to indirect obstetric causes. Despite progress in health policy and service delivery infrastructure, Kenya's maternal mortality ratio remains high at 355/100,000 live births. In the first Kenya confidential enquiry into maternal deaths report (2017), anaemia was the second leading indirect cause of maternal mortality at 14.6 percent and Haemoglobin is screened in 72 percent of women attending antenatal care in health facilities. Disparities in maternal and neonatal health indicators exist across the counties.While the majority of maternal deaths are preventable, only one-third of public health facilities are capable of delivering the seven life-saving signal functions of basic emergency obstetric and newborn care (BEmONC). This is due to inadequate skilled human resources for health, gaps in the quality of care and inequitable geographic distribution of services.
Improving standards of quality maternal and newborn care
Achieving the SDG 3 targets will require improvements in the quality of maternal and newborn care services. The World Health Organization (WHO) defines eight standards for improving the quality of maternal and newborn care, one of which calls for “competent, motivated staff to be consistently available to provide routine care and manage complications”. Multiple factors influence health workers’ performance, including health workers’ knowledge and skills gaps, caseload, patient demand, clinical practices, educational opportunities, availability of supplies and equipment, and a quality improvement process.
Liverpool School of Tropical Medicine (LSTM) supports 21 healthcare facilities in Vihiga County through the Quality Improvement for Integrated HIV/AIDS, TB, and Malaria in the Antenatal and Postnatal (ANC/PNC) Programme (2021 – 2024). The project is funded by Takeda CSR Global through the Global Fund. The project aims to reduce maternal and neonatal mortality and morbidity through capacity strengthening of healthcare workers in ANC/PNC service delivery, quality improvement (QI) using standard-based audit (StBA) and mentorship.
Esiarambatsi Health Centre is one of the facilities supported by the project and is implementing StBA to improve quality of care in ANC/PNC services. Following the training of ANC and PNC healthcare workers on StBA in March 2023, a multidisciplinary QI team, consisting of 12 members from all the facility’s departments was formed. This QI team is chaired by the facility in charge and conducts monthly meetings to review the progress of quality improvement initiatives applying the StBA steps.
Prioritization of screening for anaemia in pregnancy
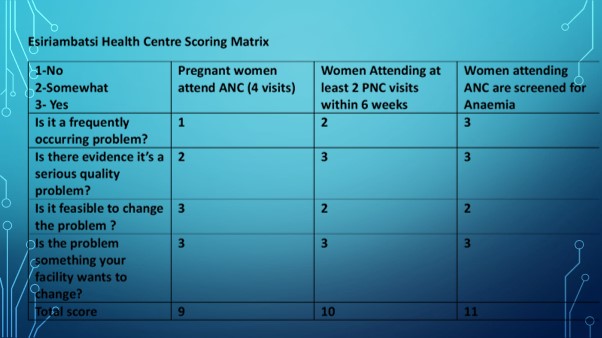
During the second meeting held in April 2023, the team identified three key challenges facing the facility: Low number of pregnant women attending at least 4 ANC visits, low number of women attending postnatal check-ups at 2 weeks, and low proportion of women screened for anaemia in pregnancy. Using a prioritization matrix, low screening for anaemia in pregnancy emerged as a priority problem which was linked to MNH QOC standard 1.2.4 All women attending ANC are screened for anaemia and if anaemic treated.
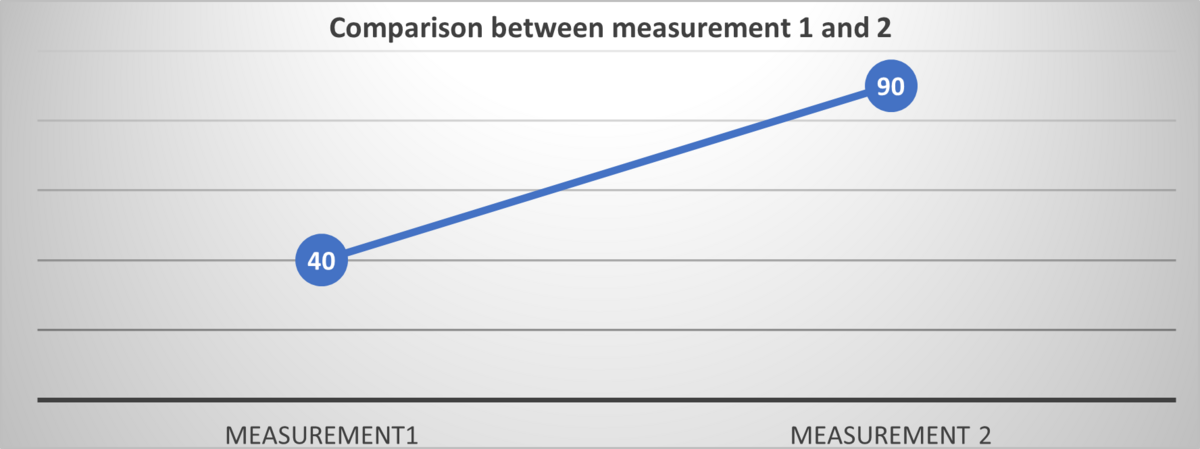
Measurement 1: Baseline assessment
Measurement one aimed to assess current practices before interventions were made. The data was collected retrospectively for three months to measure the standard 1.2.4. The team reviewed the mother-child booklets and laboratory registers for the three baseline months (April to June 2023) using a standardized data collection tool 1.2.4. Data was collected from a sample of 50 women attending ANC clinic in July 2023. The team then analysed the data.
Feedback, identifying changes needed and implementing changes
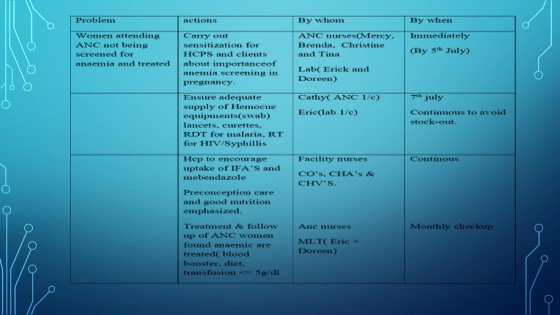
The findings were disseminated to the facility team for buy-in. The findings showed that only 40% (n=20) of women attending ANC were being screened for anaemia. Root cause analysis revealed that there was inadequate preconception care, frequent stockouts of reagents in the laboratory, and lack of job aids for anaemia screening and treatment in the ANC. A target was set to screen at least 80% of pregnant women attending ANC at the facility.
The following actions were established and implemented to reach the target: (i) screening all women attending ANC for anaemia, (ii) providing health education on nutrition and balanced diet, (iii) improving pre-conception care, (iv) maintaining sufficient stock of cuvettes and reagents, (v) administering iron and folic acid supplements to women with haemoglobin levels below 11g/dl, and (vi) documenting test results in the women's ANC booklet and laboratory registers. The implementation process took three months.
Measurement 2: Post-implementation assessment
After three months of implementation, measurement 2 was taken for three completed months (October, November, and December 2023) using the same methodology, data collection tool, and sample size as the baseline. The findings showed an improvement in the proportion of clients screened for anaemia in ANC from 40% to 90% at measurement 2. Although this was above the set target (80%), the aim is to achieve 100% of all women attending ANC screened for anaemia in pregnancy.
Conclusion
Standards-based audits and intervention cycle was effective and resulted in improved proportion of women screened for anaemia in pregnancy. Application of this QI approach has the potential to improve the coverage and quality of care for women seeking pregnancy and childbirth services leading to better maternal and newborn health outcomes. Additional investments are needed to scale up StBA interventions to close the gap between coverage and outcomes for maternal and newborn health.