
Authors:
Martin Eyinda, Technical Officer – Liverpool School of Tropical Medicine (LSTM) Kenya
Irene Nyaoke, Senior Technical Officer - Liverpool School of Tropical Medicine (LSTM) Kenya
Duncan Shikuku, Senior Technical Officer - Liverpool School of Tropical Medicine (LSTM) Kenya
Onesmus Muchemi, Technical Officer – Liverpool School of Tropical Medicine (LSTM) Kenya
Rael Mutai, Regional Technical Advisor- Liverpool School of Tropical Medicine (LSTM) Kenya
Helen Allot –Technical Specialist - Liverpool School of Tropical Medicine (LSTM) United Kingdom
Charles Ameh, Professor Global Health, Head Emergency Obstetric and Quality of Care Unit, Liverpool School of Tropical Medicine (LSTM) United Kingdom
Introduction
Kenya's maternal mortality ratio stands at 355 deaths per 100,000 live births. This is still far from reaching the SDG target of 70 per 100,000 live births by 2030. Liverpool School of Tropical Medicine (LSTM), supported by funding from Takeda Global CSR program through the Global Fund is strengthening the capacity of healthcare workers in 21 facilities in Vihiga County to monitor quality improvements in antenatal and postnatal care. The capacity strengthening aims to improve the healthcare workers’ knowledge and skills in providing quality holistic antenatal and postnatal care for improved maternal and neonatal outcomes.
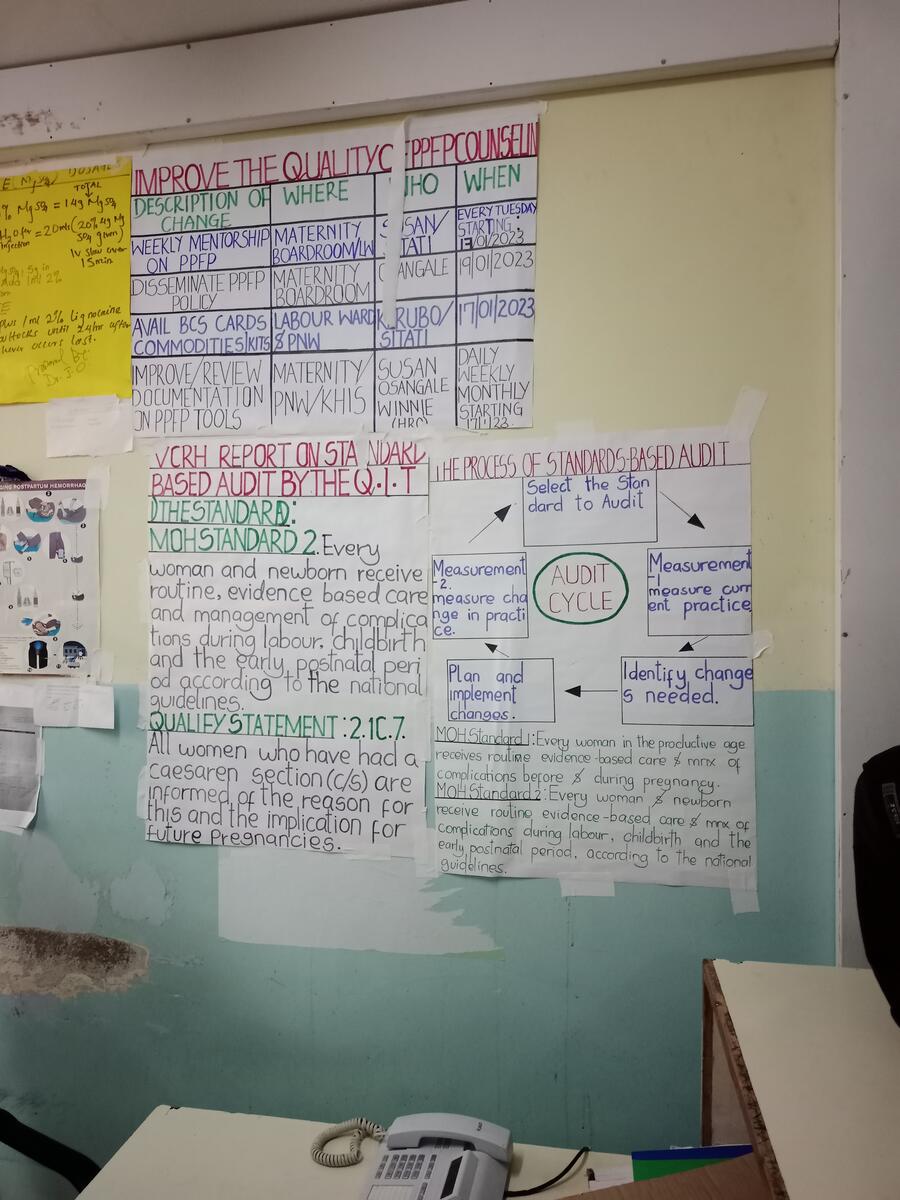
In December 2022, LSTM conducted a 3-day training for 30 healthcare providers selected from 21 project-supported health facilities in Vihiga County on a Quality Improvement package. The participants were taken through a step-by-step process of implementing a standard-based audit (SBA) using the Ministry of Health Kenya Maternal and Newborn Health (MNH) standards launched in 2022. Following the training, each participant, in liaison with their facility Quality Improvement Team (QIT) was asked to identify a quality gap in antenatal and postnatal care at their respective health facility, develop and implement the specific actions to address the identified gap build by utilising the MOH MNH QoC standards.
Step by step implementation of Standard Based Audit for Quality Improvement
Step1: Selecting Standard to Audit
Wilson Onsangale a nurse at Vihiga County Referral Hospital (VCRH), is one of the healthcare providers (HCP) trained by LSTM in Quality Improvement. After the training, he provided feedback on the training to his colleagues in the maternity department. Subsequently, the work improvement team (WIT) (departmental quality improvement team) identified several quality challenges that affect the quality of care in the MNH department. A prioritisation matrix was utilised and identified that most women undergoing Caesarean Section (CS) lacked sufficient knowledge about the reasons for their CS and the effects of the surgery on future pregnancies. The identified problem was linked to MOH MNH QOC Standard 2: “Every woman and newborn receive routine evidence-based care and management of complications during labour, childbirth, and the early postnatal period, according to national guidelines “sub-standard 2.1: “all women who have had caesarean section are informed about the reason for this and implications for future pregnancy. In 2022, 35% of all births in the hospital were Caesareans. A number of these CS cases were referrals from peripheral health facilities within the county and neighbouring counties of Kakamega and Nandi.
Step 2: Measurement 1- Baseline assessment
This entails collecting baseline data to understand the health facility’s current performance on the selected standard. A sample size of 25 women who had undergone CS were selected and consented to participate in the QI survey using an interviewer-administered questionnaire. The data collection process was completed in 5 days. The data was then analysed, and a report was generated.
Step 3: Feedback and identifying changes needed.
Following analysis of the data collected by the WIT, feedback was given to the antenatal postnatal and maternity staff. The findings showed that only 63% of women were informed about the reasons for their C/S delivery and the implication for future pregnancies. Root cause analysis was conducted to identify the reasons for the finding. Some of the reasons identified by WIT were understaffing in the maternity unit, associated with limited interaction with the clients and thus insufficient time to explain to them the reasons for the procedure. Secondly, the healthcare providers cited as a key reason as most mothers were afraid of undergoing the CS procedure and thus were not very keen to listen to healthcare providers. Finally, a communication barrier was a key challenge as some women were unable to understand the medical jargon used by health workers to explain the reasons for CS to the women.
As part of the action plan to improve awareness by women on the indications and implications of CS, the following action points for change were identified for implementation:
1. All women requiring CS were to be informed by attending healthcare providers why the procedure is needed in a language the mother can understand.
2. Bedside handover is conducted after every shift and the indication for the CS was to be clearly explained to the women.
3. Before signing the consent form, the healthcare provider verified whether the client had understood the reasons and clarified any misunderstandings on indications for CS.
Step 4: Implementing changes identified.
The Maternity and Postnatal Unit staff embarked on implementing changes proposed by the WIT as it was clear why the changes were necessary to improve the quality of care from the client’s perspective.
The implementation phase took a period of one month.
Step5: Measurement 2: Post-implementation assessment
A post-implementation assessment to evaluate any changes observed at the facility was conducted at the end of the one-month implementation period by the facility WIT. Using the same sample size of 25 clients and the same questionnaire used during the baseline assessment, data was collected for two weeks, and analysis was performed.
From the analysis, 92% of women who had undergone CS were able to explain the reasons and the implication of the procedure. Though in an ideal situation, the standard was supposed to be achieved 100%. Due to systematic challenges in the department such as inadequate staffing, the team set a realistic target of 90% though they will continue working towards achieving 100% compliance. Measurement 2 showed a 29% improvement from the baseline findings. The feedback was given to the staff. WIT appreciated the staff for their commitment and emphasised the need for the staff to continue working towards achieving 100% standard compliance and maintain it at this level of performance. The department will review the standard quarterly to monitor and evaluate progress.
Challenges encountered during the process.
There were several challenges encountered during the implementation process of the standard-based audit. These challenges were as follows:
- Low staffing in the health facility was problematic during giving feedback, it was especially difficult to get the entire team at one time since each shift has one or two staff.
- Some staff were not keen to implement the changes that were recommended, and more efforts are required to sensitize every HCP for a sustained improvement in care.
- There is inadequate space to maintain privacy when conducting the bedside handover at every shift.
- Sometimes the members of the QI team were not available, some were off duty while others were on annual leave making it difficult to get a quorum.
What worked well?
- The questionnaire used for the first and second measurements was simple, short, and easy to administer.
- Since the facility is a training institution, the team leveraged the students rotating in the department to administer the questionnaire.
- Basic data analysis including proportions was all that was required and easily performed by the hospital staff and the WIT.
Next steps
To ensure the quality of care, there is a need for quarterly assessment of the standard audited and to timely address any gaps identified. This will ensure that all women who undergo CS understand the reasons and implications of the procedure for their future pregnancies.
This collaborative programme between the MOH, LSTM and the County Government of Vihiga will support capacity strengthening of healthcare workers on Quality Improvement in ANC and PNC. A total of 90 healthcare workers are targeted for training in 2023. Secondly, LSTM in partnership with the county will continue to offer technical support to the 21 project-supported facilities through supportive supervision visits, mentorship, and quarterly QI review meetings. Lastly, the facility will apply the same methodology to continuously review quality of care by selecting and implementing priority standards in subsequent quarters, for sustained MNH quality improvements.