LSTM’s Dr Peter MacPherson, working with colleagues at the Malawi-Liverpool-Wellcome Trust (MLW) Clinical Research programme and the London School of Hygiene and Tropical Medicine (LSHTM) have completed a two-year study looking at the role AI chest X-ray screening technology for diagnosing TB in low resource settings.
The work, the results of which are published in PLOS Medicine, have already led to an update in WHO TB screening guidelines. Utilising this state-of the art, robust digital x-ray equipment and automated computer software packages enables accurate point of care diagnosis in primary care settings across sub-Saharan Africa, reducing some of the catastrophic diagnostic costs often incurred by people living with TB.
TB, one of the leading infectious killers worldwide, remains challenging to diagnose in low-resource settings, and patients frequently face multiple health centre visits at high cost before definitive diagnosis and treatment can begin. With HIV being a major risk factor for TB, already vulnerable patients are required to travel frequently, often significant distances at great personal financial costs, which often leads to late and missed TB diagnosis.
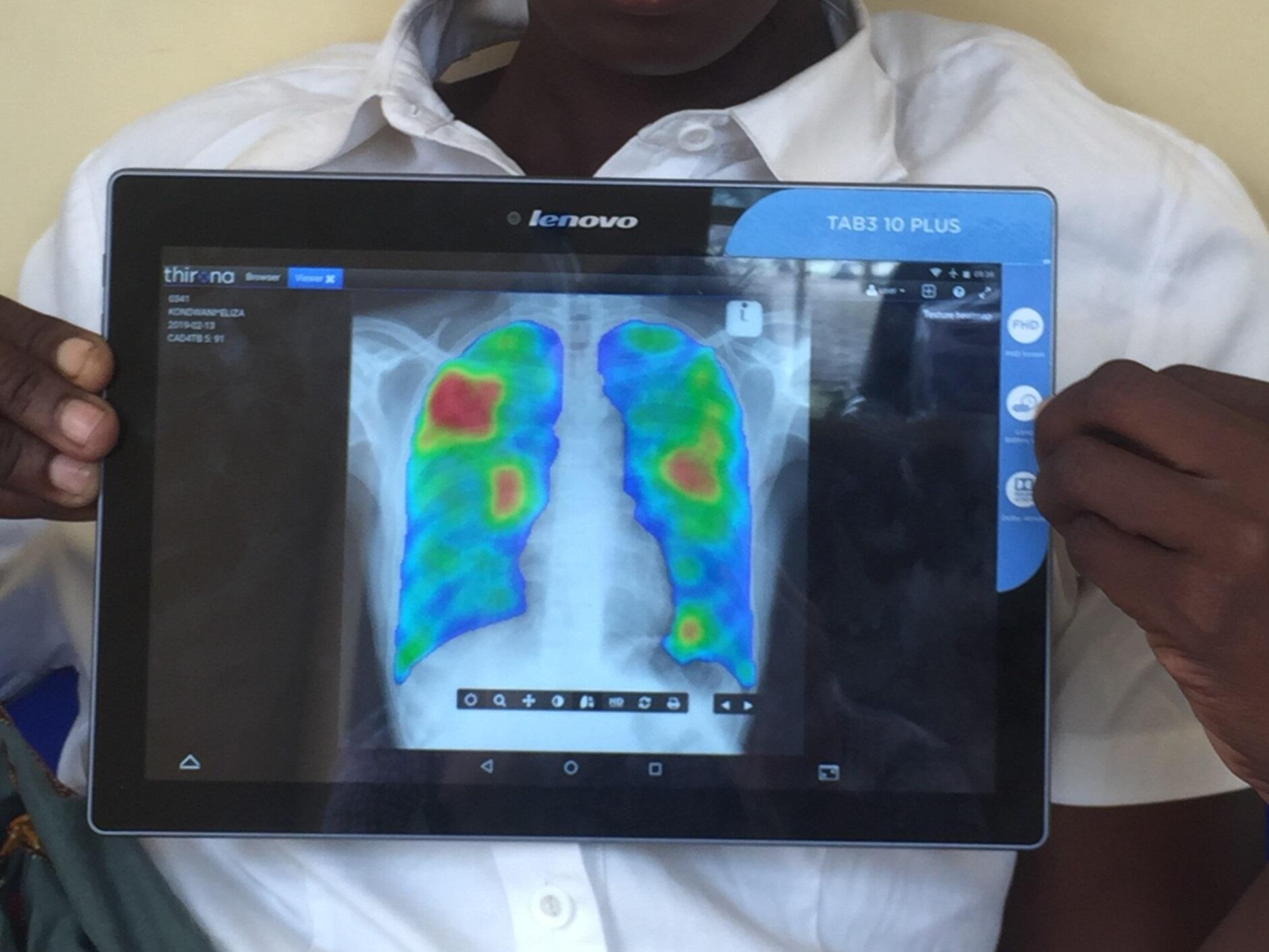
The team investigated whether offering all those attending primary care in Blantyre, Malawi HIV testing and linkage to antiretroviral therapy (ART)—either alone or combined with computer-aided digital chest X-ray (DCXR-CAD) and subsequent sputum Xpert confirmation—could improve the timeliness and completeness of HIV and TB diagnosis and treatment compared to current standard approaches. A total of 1,462 adults attending a primary clinic in Blantyre, Malawi, with cough were randomly allocated to receive either standard health worker approaches, or HIV testing and linkage to treatment with additional digital chest X-ray screening for TB interpreted by computer-aided diagnosis software, and were followed for 56 days to investigate initiation of TB treatment, missed TB and HIV diagnosis, and cost-effectiveness.
Dr MacPherson said: “We found that combining the digital chest x-ray and software interpretation with universal HIV screening led to increased timeliness and completeness of HIV and TB diagnosis. Healthworkers found the equipment easy to use and less intrusive for patients across the study areas and we believe that if implemented at scale these interventions have the potential to rapidly and efficiently improve TB and HIV diagnosis and treatment, saving lives and reducing costs in low resource settings.”
Given that the equipment is so straightforward to use, the team feel, and evidence shows, that digital radiography can be task-shifted from radiographers to other health workers, and potentially trained lay-people. This could be extremely important in settings like Malawi where numbers of radiographers are very limited. The new generation of machines are also powered with rechargeable batteries, meaning that a constant electricity supply is not necessary, so they can be used even in remote settings.
Working closely with the Malawi TB and HIV Departments in the Ministry of Health from the design of the study, through its implementation means that DCXR-CAD has already been implemented in several primary health care centres for TB screening. Dr MacPherson concluded: “Sharing these results with the Guideline Development Group for the 2021 updated WHO TB Screening Guidelines, has meant that for the first time there is now an international recommendation that DCXR-CAD can be used for TB screening.”
The team are now conducting a second trial (CASTLE Study) in Zomba Central Hospital to see whether DCXR-CAD can reduce mortality in people with HIV admitted to hospital.
PLOS Medicine: Computer-aided X-ray screening for tuberculosis and HIV testing among adults with cough in Malawi (the PROSPECT study): A randomised trial and cost-effectiveness analysis Published: September 9, 2021 https://doi.org/10.1371/journal.pmed.1003752