LSTM’s Seminar Series continued this week with a talk from LSTM’s Professor Louis Niessen. His presentation, entitled: How important is tropical medicine and international health? Research findings on disease control, wellbeing, poverty, was introduced by Professor Shabbar Jaffar, head of LSTM’s Department of International and Public Health.
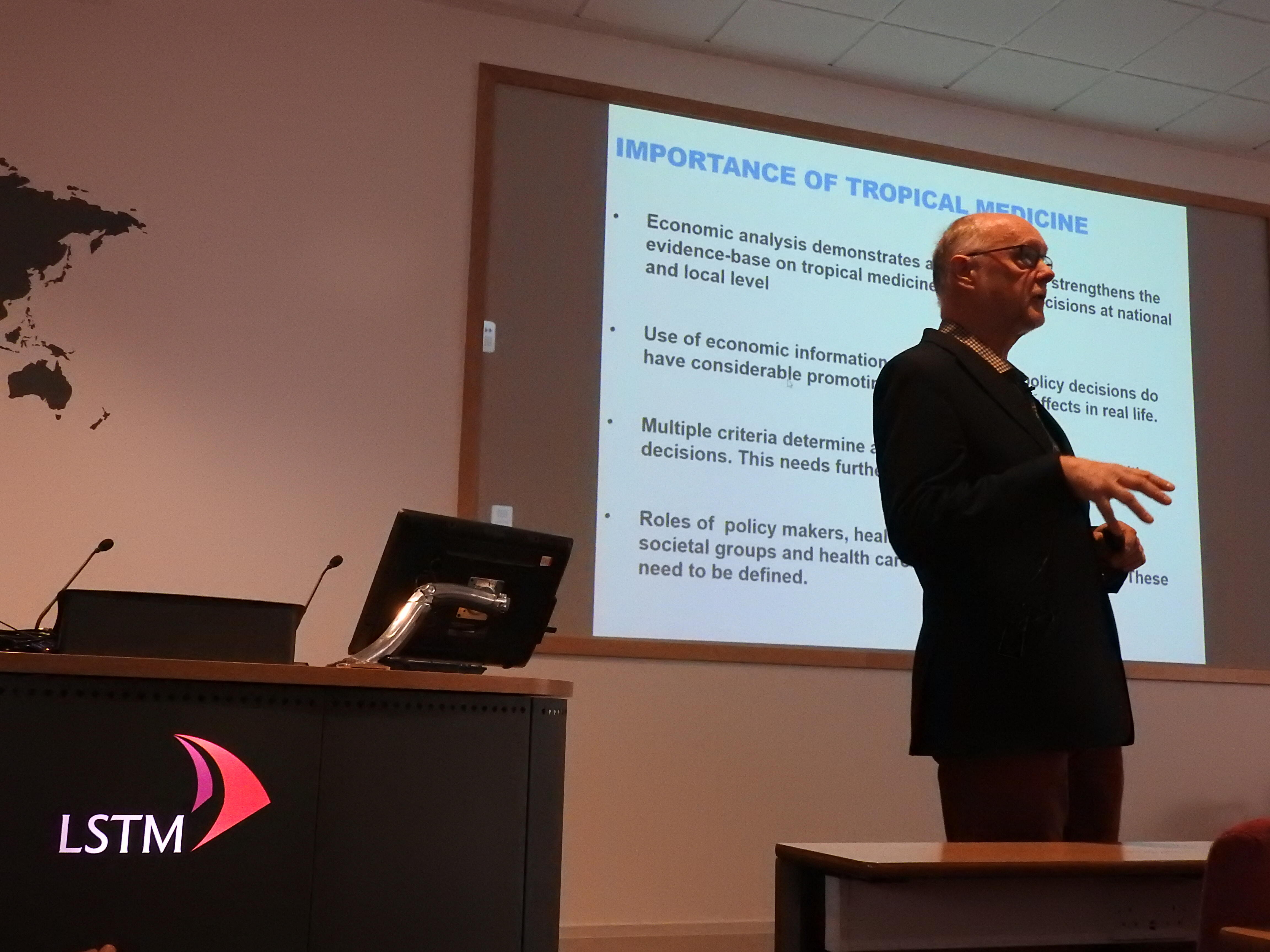
Professor Niessen began by giving a general picture of health economics, which he explained was not limited to research on appropriate resource use and interventions, but about providing evidence for the relative cost effectiveness of health intervention strategies because policy makers and funders need to know if an intervention strategy works, provides value for money, and is feasible and acceptable in real-life settings. He believes that health economics and medicine are good marriage with economic analyses demonstrating added value which strengthens the general evidence base to support policy and research decisions in tropical medicine and national and local levels.
While health and well-being is reflected in the third of the UN’s Sustainable Development Goals (SDGs), health is also central to several others. A leading SGDs theme is that of universal health coverage in all countries, which, from an economic perspective, is about balancing between efficiency and equity. These concepts, Professor Niessen explained, are interlinked: working efficiently there are more sources to promote equity. Looking at life expectancies in a cross-countries comparison, one observes a positive correlation between that and national health expenditure. He also explained that over time we appear to have become more and more efficient: at the same budget per person over time we can observe increasing life expectancies. However, as we become more successful we are to expect to start to see diminished returns in terms of mortality and morbidity reduction. We will need better and more sensitive outcome measures, considering multiple dimensions of wellbeing such as safety, financial security, autonomy, etc.
Despite all the progress in health, countries continue to miss appropriate health financing mechanisms. He used Bangladesh as an example to illustrate the impact of out-of-pocket health spending on poverty increase, with five million people falling below the poverty line due to personal health expenditure. As part of the present UN Sustainable Development Goals, Professor Niessen explained the importance of not only promoting population health, but also equitable distribution of health, looking at the distribution across socioeconomic and other disadvantaged groups. Historically we have seen priorities move from opinion-based, to evidence-based policy making and, now, to value-based processes.
After explaining the rationale for economic evaluation, he gave examples of systematic economic reviews and research looking at four different NTDs and their management, and looked at the socioeconomic benefit to individuals of preventative chemotherapy (mass drug administration) in the control of seven NTDs, and on the clustering of poverty and diseases.
Professor Niessen then concluded by high-lighting the impact of health economics research on evaluation of disease control strategies: it allows funders to see value for money, achieve outcomes such as increased coverage and enhanced efficiency and equity. In this way, economic evidence enhances better national and international policies in social and health programming.
You can view a recording of the seminar here.