New research seeks to better understand where and how Escherichia coli is acquired, enabling more effective interventions to prevent transmission and to help tackle the growing problem of antimicrobial resistance (AMR).
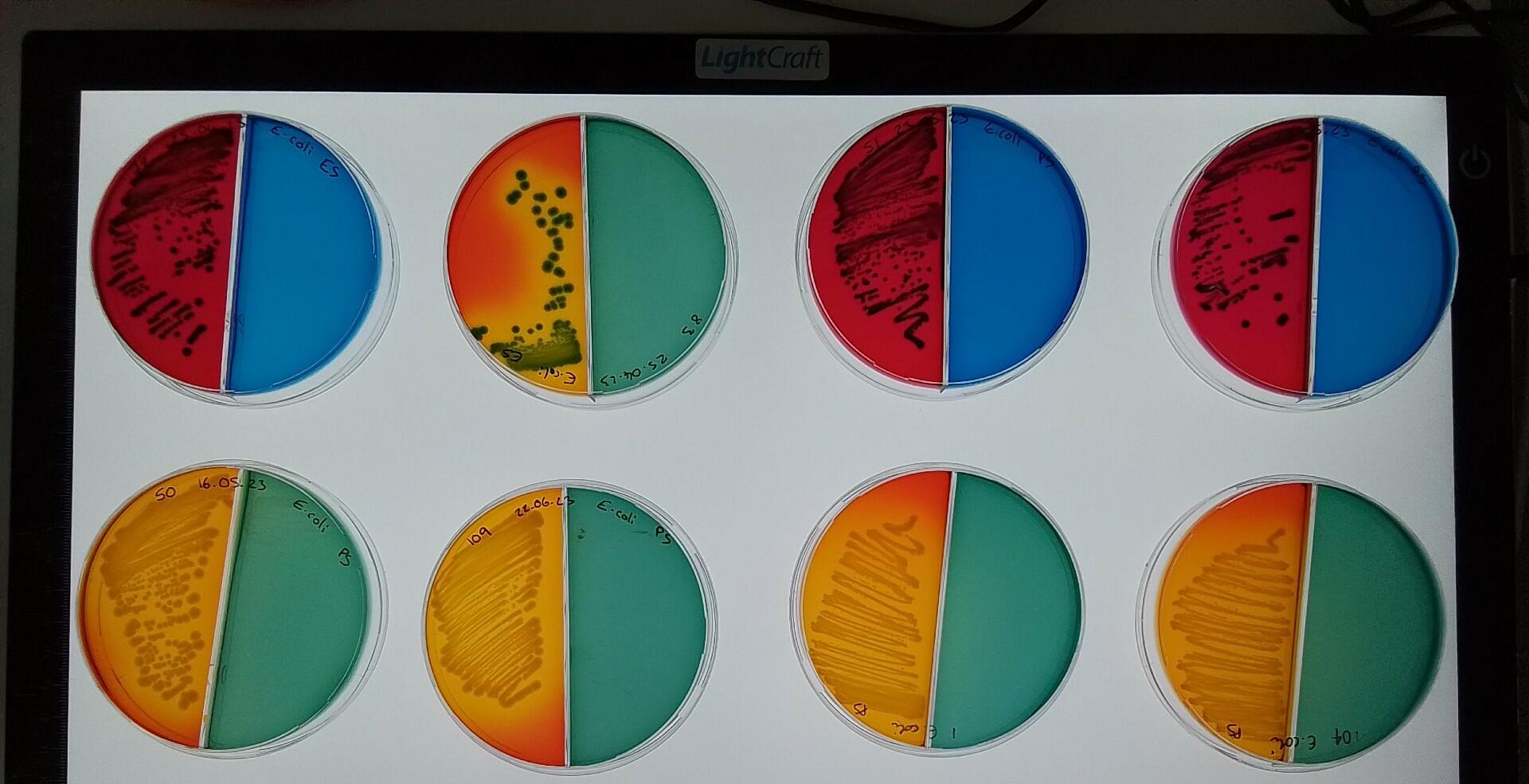
DECODE, (Defining E. coli Diversity in Complex Samples: Methods for Surveillance & Transmission), a new study led by Dr Fabrice Graf and Professor Nicholas Feasey from the Liverpool School of Tropical Medicine, will develop the microbiological methods necessary to understand the within-species diversity of E. coli from different samples such as stool, wastewater or freshwater.
The bacteria E. coli is usually harmlessly carried in the human gut, though some strains can cause serious infection, and E. coli is a leading cause of urinary tract and bloodstream infections globally, which is often complicated by resistance to antibiotics.
The new project is supported by the MRC under the framework of the JPIAMR – Joint Programming Initiative on Antimicrobial Resistance, and has launched during World AMR Awareness Week. LSTM will work alongside partners from the Fraunhofer Chalmers Centre in Sweden and the University of KwaZulu-Natal in South Africa on the research.
It is anticipated that the study will have an impact on a wider scale by creating the tools to improve AMR surveillance and helping design and implement preventive measures against AMR infections in a variety of settings.
Dr Fabrice Graf, Senior Research Associate, at LSTM, said: “We are delighted to have secured funding for this important project to tackle the growing problem of AMR. We will develop surveillance tools to disclose pathways of transmission, which will help to design interventions that can reduce the number of serious, drug-resistant infections. Fewer infections will also reduce the use of antibiotics and thus the selection pressure on bacteria to evolve resistance.
“Drug-resistant infections lead to higher morbidity, mortality and costs for health systems. The burden of AMR is higher in low-resource settings, where ‘last resort’ antibiotics are often unavailable or too expensive, leaving many drug-resistant infections untreatable. Improved surveillance is key to informing infection control and prevention strategies.”