A research team from Spain has prepared a Cochrane systematic review that explores the efficacy, safety, and adherence to fixed-dose combinations (FDCs) of drugs versus single-drug formulations to treat people who are newly diagnosed with tuberculosis (TB).
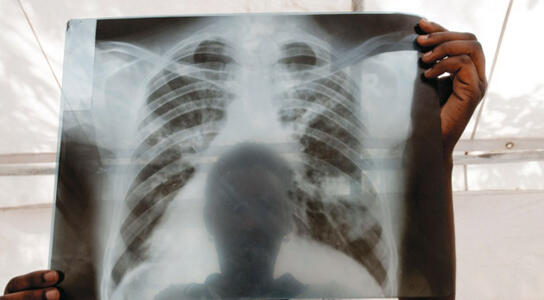
Tuberculosis (TB) is a curable and preventable disease caused by the bacterium Mycobacterium tuberculosis and most often affects the lungs of infected individuals. This disease is found worldwide, and 95% of TB deaths occur in low- and middle-income countries. Also, TB is the leading killer of HIV-positive people.
The intensive treatment for pulmonary TB is a six-month regime that consists of two months of isoniazid, rifampicin, pyrazinamide, and ethambutol, followed by four months of isoniazid and rifampicin in FDCs that are combined in one tablet, or separately as single-drug formulations. However, the duration and complexity of the treatment means patients sometimes default. Non-adherence and erratic treatment fails to cure patients and creates chronically contagious cases, which may excrete drug-resistant TB bacteria. The World Health Organization (WHO) recommends FDCs to facilitate the optimal drug treatment of TB by improving adherence, possibly reducing prescribing errors, and improving drug supply efficiency.
The review authors assessed the safety of the FDC regime, its acceptability by the patient, and its ability to treat pulmonary TB in newly-diagnosed adults versus single-drug formulations. They searched the available literature up to 20 November 2015 and included 13 randomized controlled trials with 5824 participants, and compared FDCs with single-drug formulations in adults aged 15 years or more. The included trials were published between 1987 and 2015, and included participants in treatment with newly-diagnosed pulmonary TB in countries with high TB prevalence. Only two trials reported the HIV status of included participants.
The Cochrane review found there is probably little or no difference between FDCs compared to single-drug formulations for treatment failure. However, relapse may be more frequent following treatment with FDCs, and the number of deaths were similar between the two groups. Furthermore, the review showed little or no difference in serious adverse effects or events that led to discontinuation of therapy between the two regimes. Regarding TB diagnosis, there was little or no difference in sputum smear or culture conversion.
The review authors concluded that FDCs have similar efficacy to single-drug formulations for treating people with newly diagnosed pulmonary TB.
The findings support current recommendations for FDCs for pulmonary TB.
The CIDG has been in operation since 1994. With over 600 authors from 52 countries, it is led by Professor Paul Garner, Dr David Sinclair, and Anne-Marie Stephani, and has its editorial base at LSTM.
Gallardo CR, Rigau Comas D, Valderrama Rodríguez A, Roqué i Figuls M, Parker LA, Caylà J, Bonfill Cosp X. Fixed-dose combinations of drugs versus single-drug formulations for treating pulmonary tuberculosis. Cochrane Database of Systematic Reviews 2016, Issue 5. Art. No.: CD009913. DOI: 10.1002/14651858.CD009913.pub2.