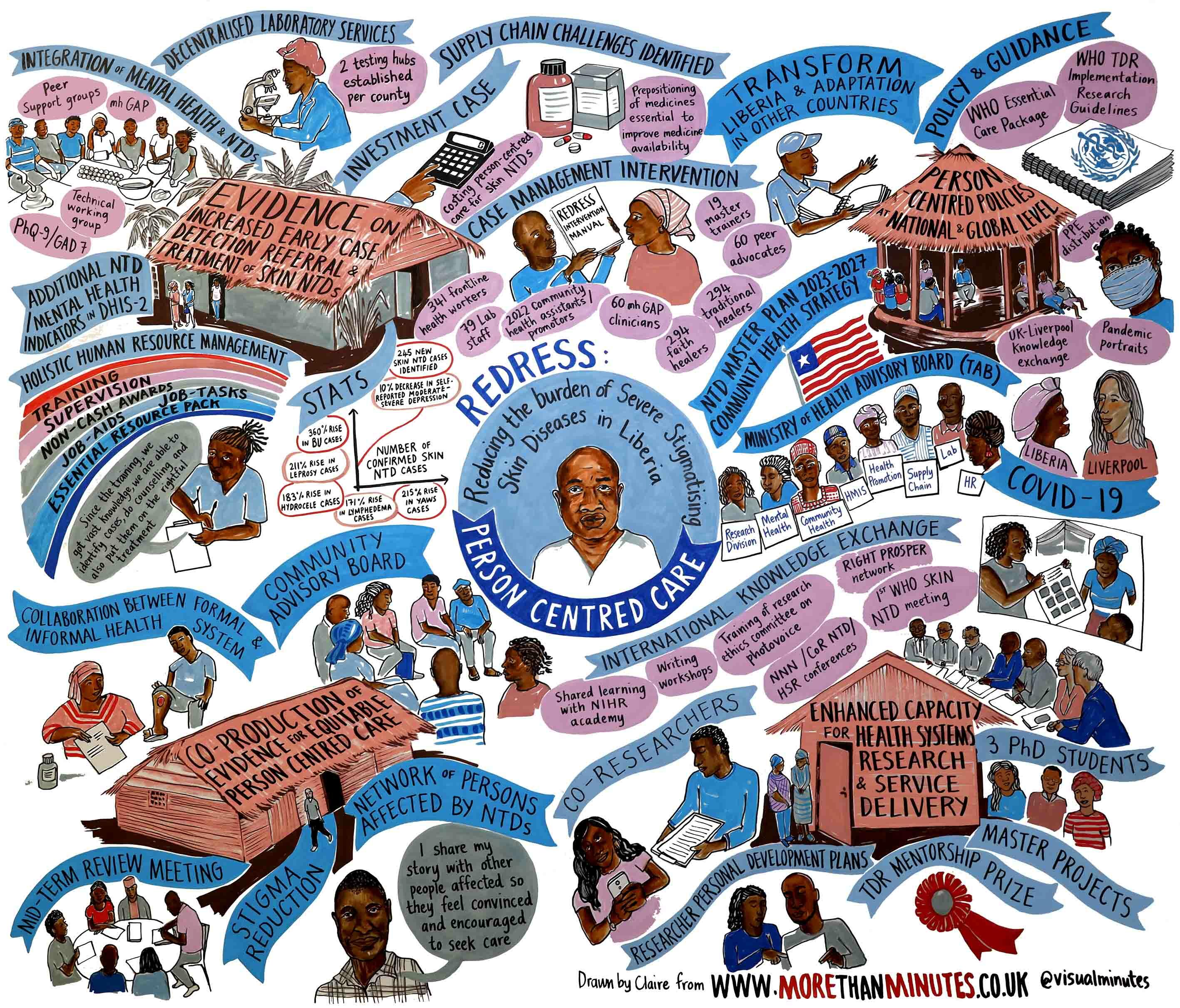
REDRESS is a £3.5 million programme awarded to LSTM from the National Institute for Health Research (NIHR) created to tackle severe stigmatising skin diseases (SSSDs), or skin Neglected Tropical Diseases (NTDs) in Liberia.
Over the last five years, REDRESS, led by Karsor Kollie, Professor Sally Theobald and Dr Laura Dean, has been working to improve care, integrate mental health support and combat marginalisation and discrimination.
Skin NTDs can have major consequences. Delays in diagnosis and treatment can exacerbate social stigma and exclusion while increasing the risk of disability and even death. While there is treatment available, it often overlooks social and psychological impacts, and doesn’t consider how treatment needs vary by age, geography, economic circumstances and gender.
REDRESS addresses these challenges through a person-centred approach, identifying, testing, and adapting health interventions for managing skin NTDs in Africa. The goal is to ensure all persons affected receive essential, effective, and affordable care, enhancing quality and equity across communities.
Two people critical to REDRESS's success are Emerson Rogers and Karsor Kollie. Here, they explain the programme's impact in Liberia.
Emerson Rogers, REDRESS Intervention Coordinator

As the National Coordinator for Case Management Neglected Tropical Diseases (NTD) at the Ministry of Health in Liberia, my involvement with the REDRESS research project stemmed from the crucial need to scale-up case management across Liberia whilst integrating mental health services with the Ministry's existing healthcare approaches.
REDRESS's aims fit this need perfectly, namely tackling stigmatising skin NTDs, reducing associated discrimination, particularly in rural communities where access to healthcare is limited, and assessing the mental health impact of these diseases is largely ignored.
The programme also allowed us to contribute to research assessing the feasibility of integrating mental health with NTD care, an approach that can be used worldwide.
From the outset, I recognised the significance of REDRESS's approach, which emphasised person-centred care. This approach is unique and involves all key stakeholders in patient identification, referral, diagnosis, and management.
One of REDRESS's most impactful aspects was the development of a comprehensive training manual. The manual equipped healthcare workers, including community health workers and traditional healers, with the necessary skills to address both physical and mental health needs of persons affected. By equipping such a wide range of people with the necessary skills to treat skin NTDs, REDRESS ensured that patients had much easier access to holistic care.
The training manual has been so successful that we are now expanding its use to more counties in Liberia. I also think the same model can be used in many other countries to improve and expand access to healthcare.
However, despite the success of REDRESS and the research undertaken during its operation, sustainability remains a challenge. Peer support groups, just one of the vital components of the programme, require ongoing support to continue their work effectively. As a Ministry, we are exploring integrating these groups into existing structures to ensure their longevity and impact.
Overall, REDRESS has significantly improved our NTD programme in Liberia, improving access to comprehensive healthcare and addressing the psychosocial needs of affected individuals. As we continue to implement the findings of the REDRESS project, we remain committed to advancing healthcare equity and reducing the burden of NTDs in our communities.
Karsor Kollie, Country Principal Investigator for the REDRESS programme

As the Neglected Tropical Disease Programme Director in Liberia, I saw the possible benefits of the REDRESS research project and how it could enhance our approach to skin NTDs. These diseases are relatively rare but have a significant impact on people who have them, often affecting some of the most vulnerable people in our society and causing long-term disabilities.
The Ministry's integrated approach to NTDs has already had good results, but there needs to be more care provided in some areas. REDRESS provided an opportunity to fill these gaps using evidence-based methods and by integrating mental health services with NTD care.
The impact of REDRESS has been enormous and visible. The project brought together a wide range of partners and stakeholders to address issues around skin NTDs. The engagement with traditional healers was particularly noteworthy, as it recognised the importance of cultural beliefs and practices in healthcare delivery.
For many, visiting a traditional healer is the first thing they do when they have a skin NTD, often avoiding healthcare facilities because of the stigma around these diseases. Ensuring that healers act as a bridge to local healthcare facilities is a new approach in Liberia and has significantly improved health outcomes for people with skin NTDs.
The impact has been huge, scaling up mental health treatment and looking at people affected in a holistic way. Based on the interactions between the programme and people with skin NTDs, it has dispelled some of the myths around skin NTDs, dealt with some of the stigmatisation, and, after receiving treatment, they've been able to integrate back into the community far more easily.
REDRESS has also brought about tangible improvements in our NTD programme, enhancing access to holistic healthcare and addressing the complex needs of affected individuals. Moving forward, we must build upon the successes of the programme, learning from its research findings and implementing them in policy and practice, as well as continuing to prioritise integrated approaches to NTD care.
In conclusion, REDRESS has been instrumental in advancing our efforts to combat NTDs in Liberia, and its legacy will endure as we work towards sustainable healthcare solutions for all.