Some men with untreated male genital schistosomiasis (MGS) may continue to shed low levels of HIV virus in their semen despite having undetectable amounts in their blood, a small pilot study led by Liverpool School of Tropical Medicine suggests. Further research is required to confirm these observations and assess if there are any implications for HIV transmission.
The pilot study of 31 participants in Malawi – the first of its kind - provides broader insight into currently unmet clinical needs and emphasises the importance of effective MGS disease management in areas where HIV and MGS are most prevalent.
Results have been published in a new paper in Scientific Reports, authored by research lead Dr Sekeleghe Kayuni, Postdoctoral Research Associate and former PhD student at Liverpool School of Tropical Medicine, and a parasitologist with expertise in neglected tropical diseases.
A small number of participants with MGS and HIV receiving antiretroviral therapy were found to have detectable HIV in their semen, but not in their blood. However, the HIV detected was at low levels, raising doubts about significance in terms of risk of transmission, particularly if shedding is sporadic or intermittent. Further studies are required to evaluate the definitive role of MGS in enhancing HIV shedding, and to investigate if it has any potential to increase infection risk.
Schistosomiasis affects over 100 million people in sub-Saharan Africa where an estimated 6 million people are living with HIV and receive antiretroviral therapy. The clinical interactions between MGS and HIV are, however, inadequately studied.
Though further studies are required, the pilot identifies the importance of better management of MGS when set against a context of efforts to reduce HIV transmission in Malawi.
This pilot study also emphasises the need to provide increased access to praziquantel, the only medicine against schistosomiasis, to better manage MGS. In so doing, this could reduce the risk of HIV being passed onto others.
Dr Kayuni said: “These are important findings in understanding the interactions between viral and parasitic infections and how to reduce the potential risk of disease transmission. Our research team firmly believes that more effective control of MGS would improve health outcomes and could contribute towards reductions in the transmission of virus in MGS/HIV-1 co-infected men, but a larger clinical study would allow us to confirm this and understand further the implications.”
Study
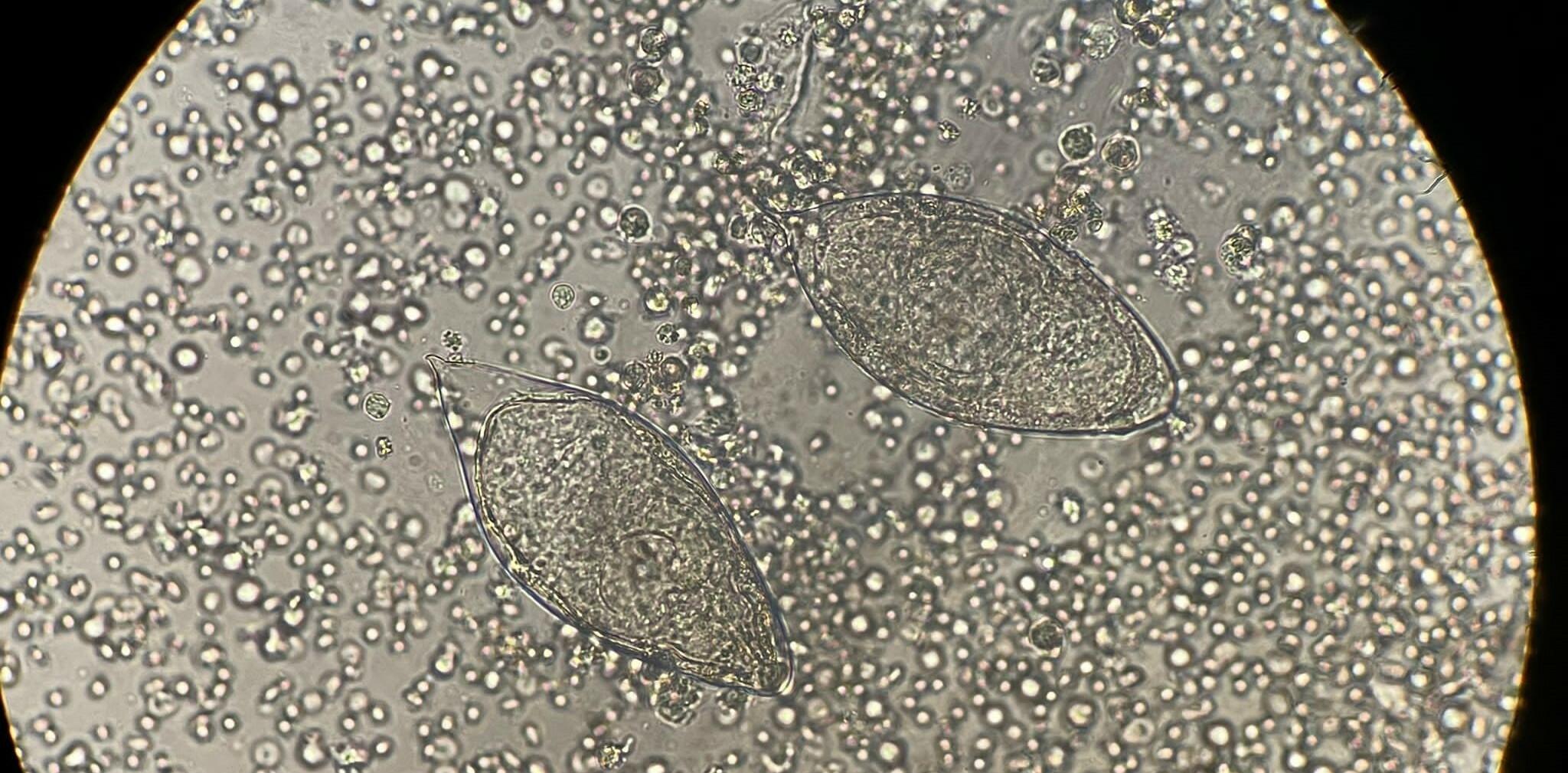
At regular intervals over 12 months, researchers analysed paired blood and semen samples from 31 men living in fishing communities near Lake Malawi - where HIV and MGS infection levels are particularly high. All participants had HIV and were receiving long-term antiretroviral therapy, with 15 also diagnosed with MGS – a parasitic infection caused by water-borne blood flukes, and 16 without.
Three participants with MGS were found to have detectable HIV in their semen but not in their blood. The two participants with detectable HIV in their semen in the MGS negative group showed corresponding levels of detectable HIV in their blood samples.
Professor Russell Stothard, Dr Kayuni’s PhD supervisor and Professor of Medical Parasitology at Liverpool School of Tropical Medicine, said: “This study is trailblazing and will encourage many clinicians not to overlook the importance of chronic MGS in effective disease management and treatment strategies. Seke put in a tremendous effort. He forged an excellent rapport with his study group that few others could have achieved.”
The full paper ‘Prospective pilot study on the relationship between seminal HIV-1 shedding and genital schistosomiasis in men receiving antiretroviral therapy along Lake Malawi’ can be accessed here.