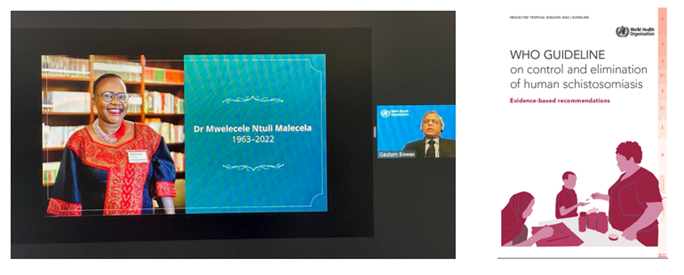
On 15th February 2022, the WHO Guideline on Control and Elimination of Schistosomiasis was formally launched. This took place with an accompanying webinar featuring supportive statements from several key health stakeholders. Video messages from several members of the Guideline Development Group (GDG) were also aired.
At the start of the webinar, we all remembered the achievements of Dr Mwele Malecela, with a moment's silence. Mwele sadly recently succumbed to cancer when in post as Director of the WHO-NTD group in Geneva. The acting Director Dr Gautam Biswas described her kind, inclusive and guiding hand behind today's guideline document. She will be much missed but remembered well.
The format of this the WHO Guideline on Control and Elimination of Schistosomiasis is just over 60 pages, with 6 Annexes. Collectively, it describes the process and outcome of the many face-to-face and online deliberations of the GDG. This guideline is unlike those before on schistosomiasis which have been based upon expert review alone. Today's guideline takes a less biased approach upon consideration of systematic reviews and more generally appraising published evidence more broadly.
In total, there are 6 main recommendations which each following judgments based upon the GRADE criteria as outlined by the following rubric:
⨁⨁⨁⨁ High quality (certainty) evidence: We are very confident that the true effect lies close to that of the estimate of effect.
⨁⨁⨁⨀ Moderate quality (certainty) evidence: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different.
⨁⨁⨀⨀ Low quality (certainty) evidence: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect.
⨁⨀⨀⨀ Very low quality (certainty) evidence: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect.
Of note, this 2022 guideline supersedes current WHO recommendations for schistosomiasis that are detailed in the 2021-2030 WHO Roadmap (https://www.who.int/publications/i/item/9789240010352). Simply put, the new intention is to better use existing control tools in more equitable ways. This is to give wider public health benefit to those infected or at-risk in future and collectively, this is an important step towards promotion of universal health coverage, safeguarding the hard-won gains made in prior schistosomiasis control.
The 6 recommendations within the 2022 guideline are:
Recommendation 1 In endemic communities with Schistosoma spp. prevalence of 10% or higher, WHO recommends annual preventive chemotherapy with praziquantel in a single dose at ≥75% coverage in all age groups above 2 years old, including adults, pregnant women after the first trimester, and lactating women, to control schistosomiasis morbidity and towards eliminating the disease as a public health problem.
GRADE: Strong recommendation; Certainty in evidence: moderate
Recommendation 2 In endemic communities with Schistosoma spp. prevalence below 10%, WHO suggests one of two approaches based on the programmes’ objectives and resources: (i) where there has been a programme of regular preventive chemotherapy, continuing preventive chemotherapy at the same or reduced frequency towards interruption of transmission; (ii) where there has not been a programme of regular preventive chemotherapy, a clinical approach of test-and-treat, instead of preventive chemotherapy targeting a population.
Grade: Conditional recommendation; Certainty in evidence: low
Recommendation 3 In endemic communities with Schistosoma spp. prevalence of 10% or higherthat demonstrate a lack of an appropriate response to annual preventive chemotherapy, despite adequate coverage (≥75%), WHO suggests consideration of preventive chemotherapy twice a year (biannual) instead of annual preventive chemotherapy.
Grade: Conditional recommendation; Certainty in evidence: Very low
Recommendation 4 WHO recommends that health facilities provide access to treatment with praziquantel to control morbidity due to schistosomiasis in all infected individuals regardless of age, including infected pregnant and lactating women and pre-schooled-aged-children under 2 years of age.
Grade: Strong recommendation; Certainty in evidence: moderate
Recommendation 5 WHO recommends water, sanitation, and hygiene interventions, environmental interventions (water engineering and focal snail control with molluscicides), and behavioural change interventions as essential measures to help reduce transmission of Schistosoma spp. in endemic areas.
Grade: Strong recommendation; Certainty in evidence: low
Recommendation 6 In communities near to the interruption of transmission, defined as having no autochthonous human cases reported for five years, WHO suggests a verification framework that consists of:
- Testing for infection in humans with a diagnostic that has high sensitivity and specificity. This process may require using a 2-step process with the available diagnostic tests starting with a high sensitivity test confirmed with a second, high specificity test.
- Testing for infection in snails as applicable with a diagnostic that has high sensitivity and specificity. This process may require using a 2-step process with the available diagnostic tests starting with a high sensitivity test confirmed with a second, high specificity test.
- Testing for infection in animal hosts as applicable with a diagnostic that has high sensitivity and specificity. This process may require using a 2-step process with the available diagnostic tests starting with a high sensitivity test confirmed with a second, high specificity test.
Grade: Conditional recommendation; Certainty in evidence: low
Common to any change in health policies and recommendations, this guideline needs sufficient time to disseminate then embed into new activities and/or realigned national strategies. No more so, perhaps than in Malawi, where new challenges in control of schistosomiasis are arising.
It is beyond the scope of this blog to make detailed comment upon all 6 recommendations. Nevertheless, Recommendations 1, 3, 5 & 6.3 have bearing on the scope of future operations of HUGS. Foremost, this coming summer we will assess the prevalence and intensity of schistosomiasis across all age bands from 2 yo onto > 45 yo, then later ascertain how quickly re-infection takes place, inclusive of any hybrid forms. We will therefore consider the application of biannual treatment when appropriate. Our hope is therefore to provide valuable policy-relevant surveillance data. Nearer the completion of our HUGS studies, we will ensure to communicate our findings to the National Control Programme Manager (Mr Lazarus Juziwelo), together with several technical experts within the WHO-AFRO/ESPEN group assigned to control and elimination of schistosomiasis.
Please watch this HUGS space!