The publication of the first report of Confidential enquiry into maternal deaths in Kenya demonstrated a disproportionate association between birth by caesarean section and maternal deaths, a finding echoed by a recent systematic review of caesarean-associated deaths and complications in low and middle income countries. These studies highlighted the necessity of improving training to enhance the quality of care surrounding operative obstetric interventions and improve decision-making to avoid unnecessary caesarean births.
To help bridge the training gaps surrounding provision of care for women undergoing operative birth, The Liverpool School of Tropical Medicine’s Emergency Obstetric Care and Quality of Care unit had developed a five-day interactive course, designed to enable participants to provide holistic, evidence-based, skilful, and respectful care to women as they journey through a surgical birth experience.

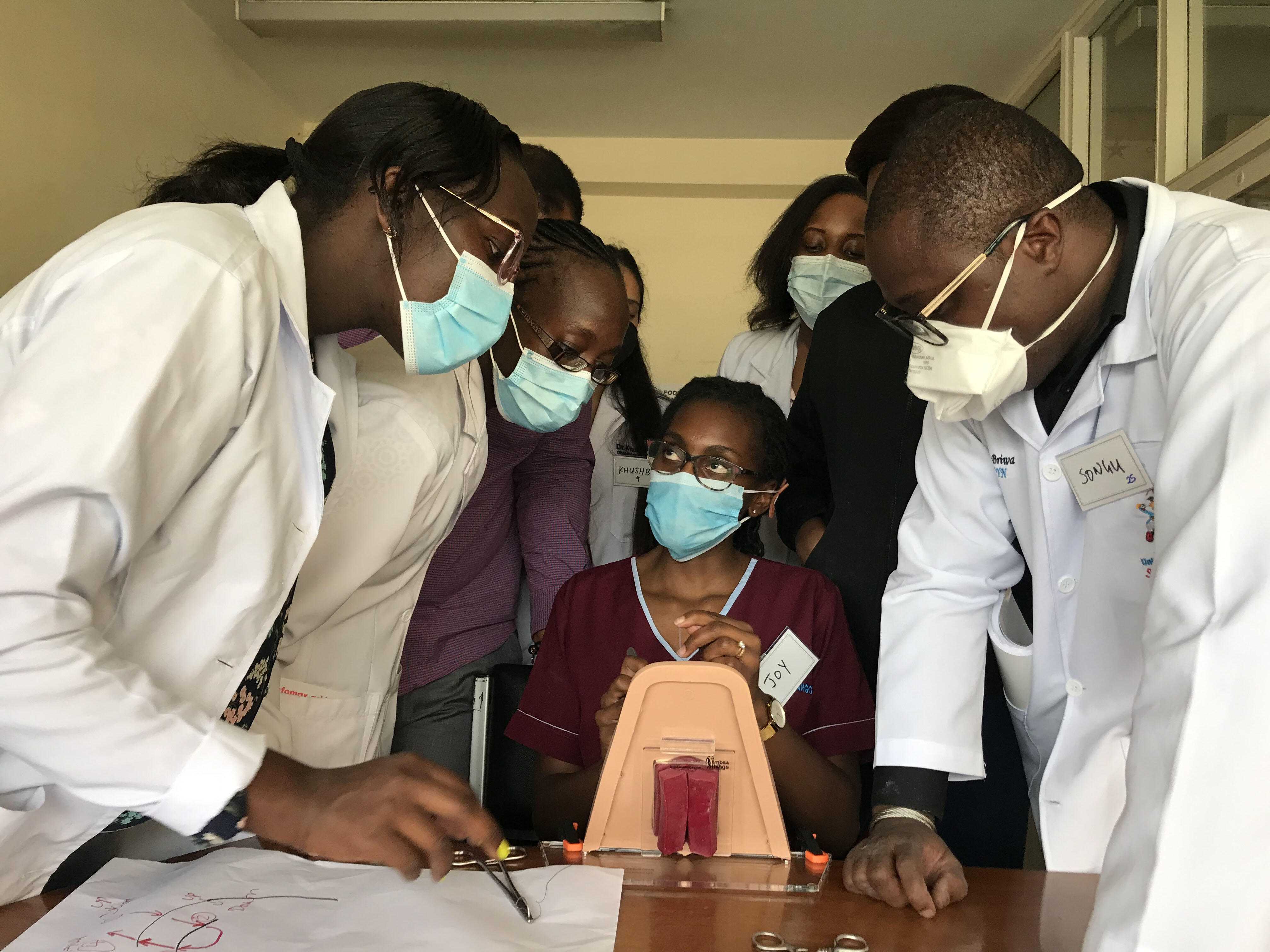
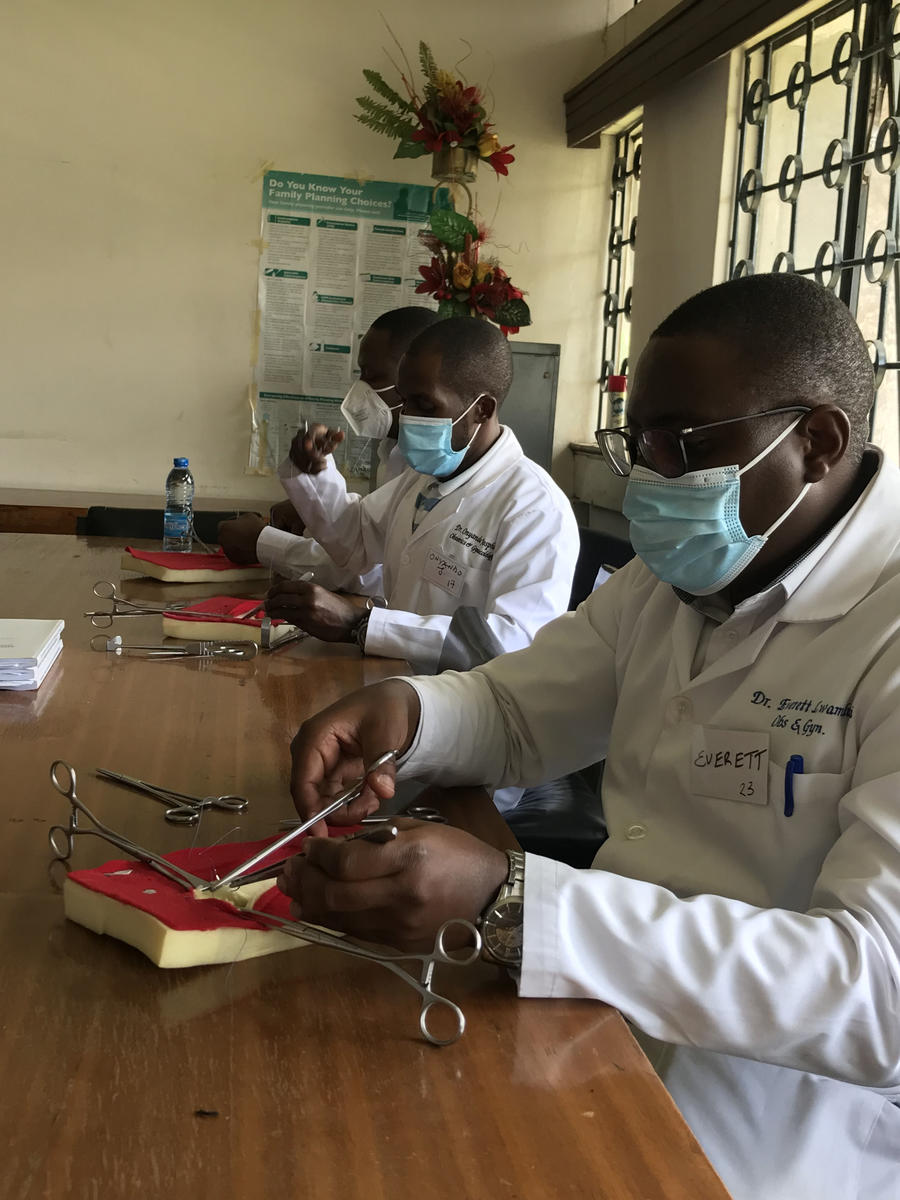
The advent of Covid-19 posed various logistical challenges and the course evolved, of necessity, into a blended learning event, consisting of three components; a self-directed learning component, now hosted on-line by the World Continuing Education Alliance, a series of virtual real-time discussion groups and an abbreviated two-day face-to-face component focusing purely on skill acquisition.
Ensuring sustainability of the training is key to on-going quality of care improvement. We have implemented this training package using the face-face format before 2020 and thereafter using the blended learning approach to train medical doctors, obstetricians, anaesthetists, and perioperative nurses in Kilifi, Taita Taveta, Usain Gishu, Vihiga and Garrisa. To ensure sustainability of this approach, we proceeded to embed this within the obstetric post graduate training programme at the University of Nairobi. In 2022, we trained an entire year-group of 93 residents at the University, coupled with training 15 of them as trainers we jumped at the chance. The new trainers will continue to train their colleagues going forwards, a process that has already started with the trainers teaching other residents on-line, supported by experienced mentor-trainers.
Although still early days, already we have received anecdotal reports of changed clinical practice, with post-caesarean hysterectomies avoided and lives saved by the use of uterine compression sutures and condom-catheter balloons for cases of post-partum haemorrhage, and assisted vaginal births by vacuum being performed where previously a difficult second stage caesarean would have been undertaken.
Local support is essential, and the training has been very well received by senior members of the Department of Obstetrics and Gynaecology. Dr Diana Ondieki, lecturer in Obstetrics and Gynaecology, told us “I came to the course as a sceptic but I can see that it is really changing lives”. The course graduates have become advocates, encouraging their peers to attend, and generating an air of eager anticipation. We are grateful for the welcome by and collaboration with Professor Cheserem, Chair department of Obstetrics and Gynaecology, University of Nairobi.
For the future, we are confident that this new generation of trainers have been enabled to pass on the lessons learned from the course as they adapt to a style of delivery of the course curriculum best suited to the departmental environment. Once that pattern becomes established, we will have succeeded in our mission to render ourselves ‘redundant’ and will have “passed it on”, Sustainable Development with Aid from the British people! We will conduct a comparative study to compare the 5-day face-to-face training to the blended training approach.