LSTM Centre for Tuberculosis Research
To improve health, social and economic outcomes for people affected by tuberculosis (TB) through research, partnership, and education
Tuberculosis is an infectious disease of public health significance, disproportionately affecting the most vulnerable populations globally. These vulnerable groups are characterized by a heightened risk of tuberculosis disease, and their disadvantaged or marginalized socioeconomic status hinders their access to the healthcare system
The Political Declaration of the 2023 UN High Level Meeting on the fight against TB renewed the hope, momentum and political commitment at the global level to end TB.


The LSTM Centre for TB Research takes a unique approach to tackling tuberculosis, seamlessly transitioning from field-based investigations to laboratory research and back again. This trajectory ensures that their discoveries quickly translate into real-world solutions for those battling the disease.
World-Class expertise in TB research with a global reach:
- Global Network: LSTM has a worldwide team of leading experts, spanning every stage of the TB care pathway, from discovery to delivery.
- Diverse Settings: Their research takes place in a variety of geographical settings, ensuring their solutions are applicable to different contexts.
- Cross-Disciplinary Approach: LSTM's strength lies in its collaborative spirit, bringing together specialists in diagnostics, pharmacology, drug development, immunology, clinical services, trials, social sciences, statistics, epidemiology, modelling, health economics, implementation science, evidence synthesis, policy, and diplomacy.
A translational pipeline for impact:
- Fieldwork Focus: LSTM starts by understanding the challenges faced in communities affected by TB, ensuring their research addresses real-world needs.
- Laboratory Insights: In the lab, researchers delve into the biological mechanisms of TB, paving the way for new diagnostics, treatments, and prevention strategies.
- Back to the Field: LSTM actively collaborates with global partners to implement their research findings in communities, building local research capacity and improving healthcare systems.
Disseminating knowledge, empowering communities:
- Knowledge Sharing: LSTM actively shares their scientific knowledge with local partners, fostering a culture of research and innovation in areas with the highest TB burden.
- Capacity Building: They invest in training and mentorship programs, empowering local researchers and healthcare workers to take ownership of the fight against TB.
By combining world-class expertise, a global reach, and a commitment to community engagement, we are bridging the gap between science and action.
Our research impact in TB diagnosis, treatment and care
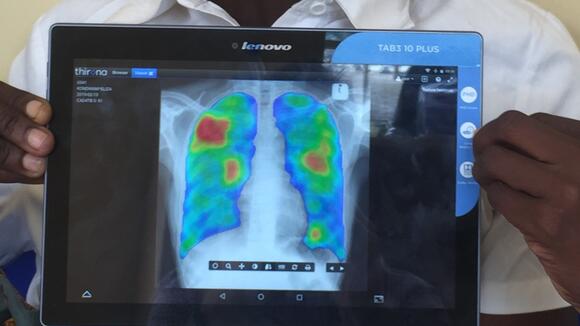
LSTM's pioneering research has empowered healthcare systems to combat MDR-TB more effectively across multiple fronts. Simulation modelling allows for optimized diagnostics, research informs better treatment regimens, and innovative delivery models ensure patients receive necessary medications. These combined efforts offer a brighter future for MDR-TB management and control.
Diagnosis and access to TB services
Transforming gendered pathways to health for people with TB in urban settings
LIGHT is a six-year international health research initiative supported by UK aid and led by LSTM in collaboration with partners in Kenya, Malawi, Nigeria, Uganda, and the UK. LIGHT seeks to generate fresh insights into the efficacy of diverse gender-sensitive strategies and pathways for health in urban settings with high HIV prevalence, specifically focusing on individuals with TB. The program strives to enhance health, socio-economic conditions, and equity outcomes, while also playing a crucial role in halting the transmission of TB.
A new model for trialling TB diagnostics and treatments
Setting up a TB human challenge model at LSTM
LSTM is setting up a TB human challenge model, in collaboration with the University of Oxford Accelerator Research Centre.
The model will be overseen by the Liverpool Vaccine Group (LVG), led by Liverpool School of Tropical Medicine’s Professor Daniela Ferreira, Dr Andrea Collins, and Dr Ben Morton, and will use live intradermal BCG vaccine (a TB specific vaccine) as the challenge agent.
BCG is given to healthy volunteers and skin punch biopsies are taken two weeks later, to isolate BCG by culture and PCR (polymerase chain reaction), which copies small segments of DNA. The team will also be investigating minimally invasive methods of skin sampling to allow long-term monitoring of BCG growth and the immune response of the person involved in the trial.
Working with Professor Stephen Gordon(link is external)(opens in a new tab), other LSTM, and Malawi Liverpool Welcome Trust. (MLW) researchers, the team is setting up a fluorescent BCG model to allow in vivo monitoring. The model will be transferred to Malawi as it is important that TB human challenge models take place in areas with high a TB burden. This research has been made possible by iiCon(link is external)(opens in a new tab) funding.
BCG is the only existing vaccine for TB but unfortunately has limited effectiveness against pulmonary TB, the most common form, which is responsible for onward transmission. TB treatment, although improving, still requires lengthy drug combinations, which can have toxicities; drug resistant TB is an increasing public health crisis. Unfortunately, current phase three vaccine and drug trials for TB are large, prolonged, and costly. A human challenge model could be used early in clinical development to select the most promising preventative and therapeutic candidates for phase 2/3 trials, accelerating TB vaccine and drug development. We desperately need effective, low side-effect, shorter course TB treatments and a safe, effective TB vaccine is a global priority.
Our aim is for this human TB challenge work to rapidly propel us towards the WHO’s End TB Strategy to reduce TB incidence and deaths by 80-90% respectively by 2030.
Building capabilities to enhance the diagnosis of tuberculosis: Start4All
Start4All is a four-year, US$15m Unitaid funded project focused on global improvement of TB screening, diagnosis, and treatment. Through identification and evaluation of existing and novel combinations of diagnostic tests, with a range of populations and at multiple health system levels Start4All is committed to increasing equitable access to timely detection of TB and linkage into quality care and treatment for all.
Project activities include work in seven partner countries with high TB burdens (as identified by WHO): Bangladesh, Brazil, Cameroon, Kenya, Malawi, Nigeria, and Vietnam. In collaboration with in-country partners from prominent institutions and linked with international partners including the WHO Global TB Programme, the project is well positioned to draw on existing close ties with the communities served, and a wealth of knowledge and expertise relating to the specific type of TB burden in each setting; be it TB in the general population, HIV-associated TB, or drug resistant TB.
Implemented by Liverpool School of Tropical Medicine (LSTM), as lead organisation, alongside global health advocacy partners (Unitaid & the StopTB Partnership) this multi-partner, multi-site collaboration aims to close the TB diagnostics and treatment gap, influence & strengthen partnerships at national and global level, improve scalability and sustainability of testing, expand coverage and access to affordable and equitable TB care.
IMPACT TB is a project to find and treat cases of TB in communities in both Nepal and Vietnam
In Vietnam, we are expanding a successful case finding project to six districts of Ho Chi Minh City. This is the largest city in Vietnam, a densely populated dynamic and rapidly developing city with a high proportion of economic migrants. In Nepal, we are implementing our case finding activities in four districts with a high burden of undiagnosed TB cases to reach those who do not have good access to healthcare.

In both countries, we will test different implementation models to find the cheapest way to scale-up active case finding of TB nationwide. We are working closely with the National TB Programme of each country to ensure our work complements other research being carried out and informs future policy. We will evaluate the health economics of each strategy from both a patient and a health system perspective, while also using mathematical modelling to understand both the short and long term effects on the epidemic of each strategy.
IMPACT TB will implement intensified TB case finding in four districts of Nepal Chitawan, Makawanpur, Mahotari and Dhanusha.
Visit the IMPACT TB website for more information.
DrOTS Nepal
In rural Nepal, the biggest challenge for healthcare delivery is the lack of an effective transport infrastructure. Healthcare workers or patients often walk for many hours to reach services and essential supplies are often out of stock.
DrOTS Nepal is designed for the early and rapid diagnosis of new TB cases in Pyuthan through the utilization of drones and smart pillboxes, called MERMS (Medication Event Reminder-Monitors), to support overcoming the access barrier in remote geographically isolated areas and improve treatment adherence/patient compliance. Our network of female community health volunteers use the drones to transport the sputum samples of people with TB symptoms to our laboratories or GeneXpert testing hubs.
Visits the DrOTS Nepal website for find out more.
The social and emotional burden of TB stigma
ASCOT: Addressing the Social Determinants and Consequences of Tuberculosis in Nepal

The World Health Organization's 'End TB Strategy' advocates social and economic (socioeconomic) support for TB-affected households. Despite preliminary evidence from middle-income Peru, there is no evidence for socioeconomic support for TB-affected households in low-income countries.
To address this, we developed a locally-appropriate support intervention for TB-affected households in Nepal, a low-income country with a high TB burden, The primary aim of the ASCOT pilot trial was to use mixed methods research to evaluate the feasibility and acceptability of the co-designed socioeconomic support package for TB-affected households in Nepal and generate robust evidence on a locally-appropriate, socioeconomic support intervention for TB-affected households in Nepal and inform a large-scale ASCOT trial, which will evaluate the intervention’s impact on catastrophic costs mitigation and TB outcomes.
Post-TB lung disease
Between 20-50% of individuals treated for TB experience persistent lung health issues and other disabilities, stemming either from the treatment itself or the TB infection. These lingering challenges can significantly affect the health and overall well-being of individuals even after they have been declared "cured" from TB.
Our research has been published in papers outlining the disease burden in Malawi and the broader disabilities associated with it. Taking a lead, we have published the initial clinical standards for post-TB health and well-being and are actively advocating for their implementation.
We play a crucial role in international post-TB symposiums, contributing to the dialogue and knowledge exchange on this pressing issue. However, there remains a critical need for further global research to comprehensively understand the impact of post-TB conditions. This includes investigating optimal treatments and care pathways, as well as determining the most effective metrics for measuring outcomes in post-TB health.
Evidence synthesis & health economics to support decision making
Advancing the management of multi-drug resistant tuberculosis
LSTM has contributed to WHO guidelines on the management of MDR-TB including methods of diagnosis, shortening of treatment duration and mode of delivery. It has benefitted hundreds of thousands of people in the 82 countries that have adopted the guidelines. It has also resulted in significant $multimillion cost savings for those countries’ health systems. Some countries - including Benin, Democratic Republic of Congo, Pakistan, and Nigeria - which have rolled out a primarily home-based, fully oral MDR-TB treatment using a WHO-supported operational research package to which LSTM contributed, are expected to see further savings for patients and health systems.
The WHO Operational Handbook on Tuberculosis, Module 4: Treatment - Drug-Resistant Tuberculosis Treatment provides practical guidance on how to put in place the recommendations at the scale needed to achieve national and global impact. The consolidated guidelines are complemented by this operational handbook which is designed to assist with implementation of the WHO recommendations by Member States, technical partners and others who are involved in the management of patients with DR-TB.
LIV-TB
The LIV-TB seminar series, a collaborative initiative between the Liverpool School of Tropical Medicine and the University of Liverpool, It offers a stimulating forum for in-depth exploration of diverse topics related to tuberculosis. Held monthly, these seminars feature presentations by leading researchers and group members, fostering vibrant discussions and disseminating the latest advancements in the field.
The sessions are relevant to researchers and professionals involved in tuberculosis research, control, and public health and doctoral students.
Tackling TB Morbidity
TB is a consequence of interactions between the host and pathogen. The TB Morbidity group investigates immune mechanisms by which Mycobacterium tuberculosis causes disease, with a focus on people at greatest risk of poor outcomes, to improve diagnostics and treatments. This includes the role of comorbidities (including HIV infection) and the long term consequences of TB. Current projects include a Medical Research Foundation-funded collaboration with Catholic University of Bukavu to study the genomics of drug-resistant TB is South Kivu, DRC and a longitudinal study of immune responses during treatment for HIV and TB in Malawi.