World TB Day 2020
It’s time to prevent TB to end TB #ENDTB #ItsTimeToEndTB #WorldTBDay
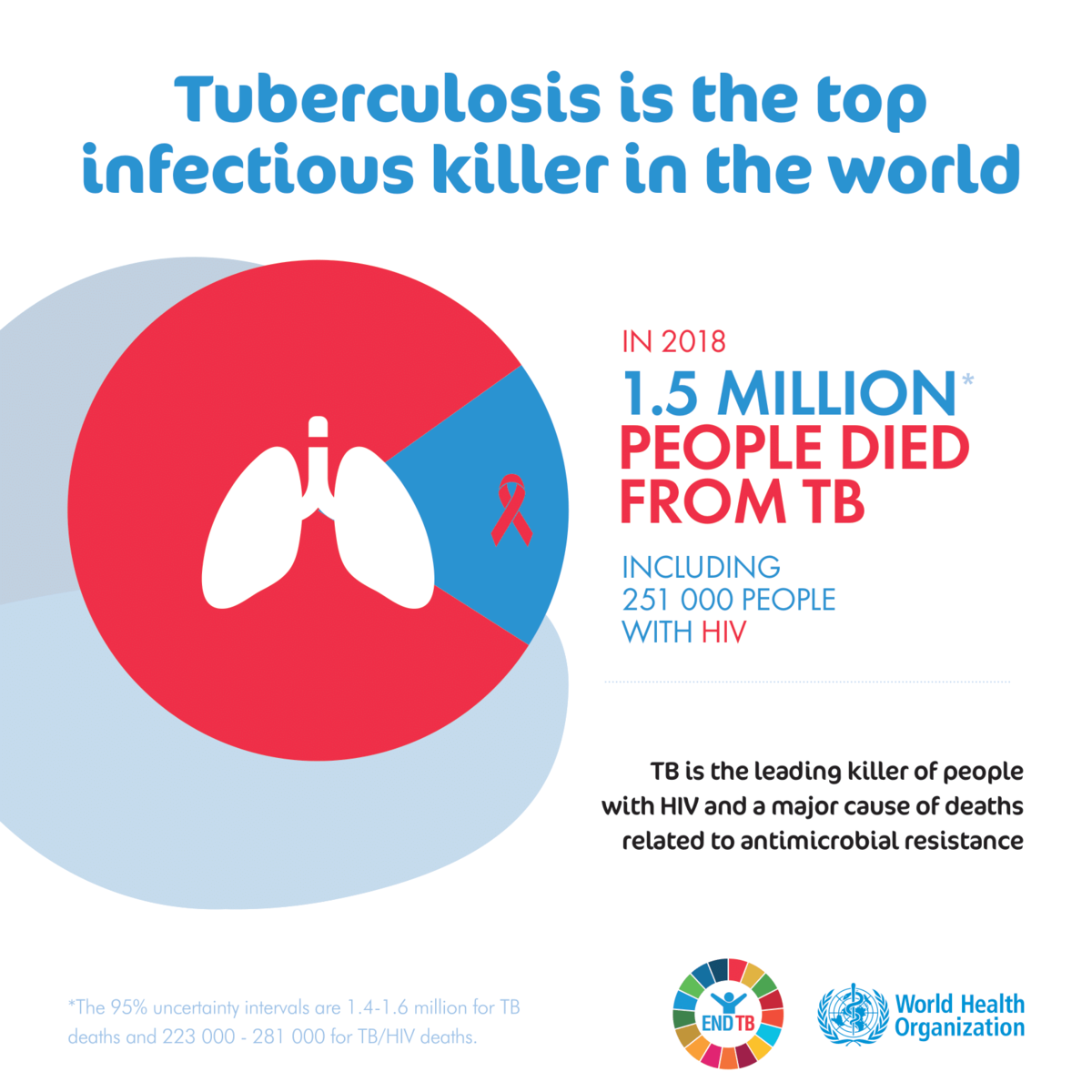
TB is a primary threat to current and future global health. In 2017 WHO estimates revealed that TB is the world’s deadliest infectious disease (affecting 10 million people and causing 1.6 million deaths) and the source of one-third of global anti-microbial resistance (AMR) deaths.
LSTM’s research covers the full spectrum of the complex, often poverty-driven, global problems around chronic lung diseases, respiratory infection and TB. It aims to reduce infection, improve prevention and optimise treatments.
The causes of these problems are complex, very often rooted in poverty, and include infections such as Mycobacterium tuberculosis and Streptococcus pneumoniae, and noncommunicable conditions such as asthma and chronic obstructive pulmonary disease.
The solutions require multi-disciplinary collaborations aimed at both prevention and management of the full spectrum of communicable and non-communicable lung conditions.
LSTM’s expertise right across the translational science spectrum, including social science, clinical & public health, health systems, and health economics, to engagement with policymakers and guideline development is deployed in collaborations to develop relevant solutions.
With key expertise in lung health and tuberculosis, LSTM hosts an especially strong TB focussed global research portfolio. Over the last five years alone, LSTM has won 30 research grants in TB with a value of over 26.7 million pounds.
These include IMPACT TB, focussed on active case finding; StopTB/HIV at one, focussed on diagnostic approaches and IMPALA, focussed on generating new multi-disciplinary evidence for high-burden lung health diseases.
LSTM also currently manages the Health Economics component of the STREAM trial of shorter MDR-TB regimens, the largest ever trial of its kind. We are looking forward to starting a new programme of work funded by the Department for International Development on improving access to TB services for men in Africa. Currently undetected and untreated men with TB account for two-thirds of TB transmission in Low and Middle-Income Countries.
Despite the commitment to ambitious global targets to end the TB epidemic by 2035, progress remains slow, and a step-change in TB research and implementation is urgently required. The 2018 UN Political Declaration “United to End TB” commits to the detection and treatment of 40 million TB cases by 2022.
It’s Time to end TB!
Some of the recent research and activities in the field of tuberculosis by LSTM teams:
Prevalence and risk factors for latent tuberculosis infection among household contacts of index cases in two South African provinces: Analysis of baseline data from a cluster-randomised trial
In this paper, published this week, researchers at LSTM studied whether household contacts of HIV-positive people with active TB in South Africa were less likely to have evidence of TB infection than contacts of HIV-negative people with TB
They found a very high prevalence of TST-positivity in household contacts in Free State and Limpopo, but especially in Mangaung, Free State, and among young children aged 0-4years.
As the majority of TB infection among young children is attributable to infection outside of the household, this indicates a very high community TB transmission, despite high ART coverage.
They also found that there was a 90% probability that the odds of TST induration ≥5mm was lower in household contacts of HIV-positive compared to HIV-negative index cases.
Tuberculosis (TB) is the leading adult infectious killer in the world. In Blantyre, high rates of HIV infection and social deprivation, i.e. crowded, poor quality housing; air pollution, poverty combine to fuel TB disease rates. TB diagnosis in primary care can be challenging. Patients are often unwell for prolonged periods and may attend the health centre multiple times. The existing tests for TB are either not accurate enough, too slow and require centralised laboratory infrastructure, or too expensive for widespread implementation (GeneXpert MTB/Rif).
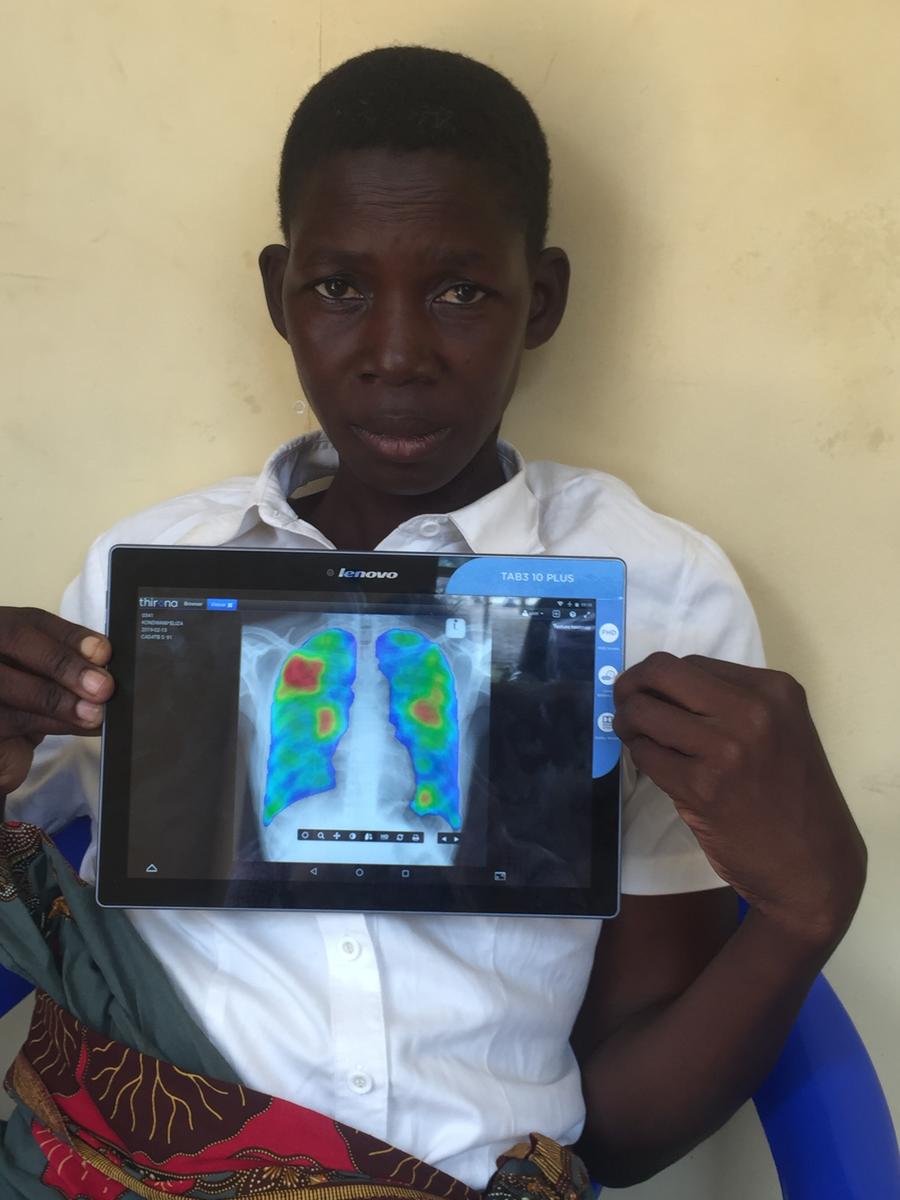
LSTM’s Dr. Peter MacPherson is based at the MLW Clinical Research Programme in Blantyre, Malawi, and leads a programme of research designing and evaluating interventions to speed up TB diagnosis using novel diagnostics to reduce the number of missed cases. This includes the PROSPECT Study, funded by the Wellcome Trust. Adults attending the Bangwe primary care clinic with cough have been rapidly screened for TB using a high-throughput digital chest X-ray. Careful monitoring of over 5000 adults entering and leaving the clinic showed that TB symptoms are very common (~30% have a cough), but very few are offered TB tests or correctly diagnosed.
The PROSPECT study has investigated if a new artificial intelligence, computer-aided TB detection programme can speed-up diagnosis. Because there are very few health workers skilled in diagnosing TB using chest X-rays in Malawi, an automated approach is needed. The CAD4TB system analyses chest x-rays for signs suspicious of TB in less than a minute, allowing health workers to focus further investigations towards the patients who most need them, and hopefully increase diagnosis rates, reducing costs, and improving patient outcomes.
Dr Samantha Donnellan: TB or not TB?
TEDxLSTM
16th November 2019
Samantha Donnellan is a Post-Doctoral Research Associate at the Liverpool School of Tropical Medicine and Winston Churchill Memorial Trust Fellow. Based at the Centre for Drugs and Diagnostic Research, Sam is developing improved methods for testing drug compounds and combinations for the treatment of Tuberculosis (TB). She collaborates with bio-engineers, researchers in the Molecular Mycobacteriology Research Unit, Cape Town and the pharmacokinetic (PK) and pharmacodynamic (PD) team at LSTM. Samantha Donnellan is a Post-Doctoral Research Associate at the Liverpool School of Tropical Medicine and Winston Churchill Memorial Trust Fellow. Based at the Centre for Drugs and Diagnostic Research, Sam is developing improved methods for testing drug compounds and combinations for the treatment of Tuberculosis (TB). She will be collaborating with bio-engineers, researchers in the Molecular Mycobacteriology Research Unit, Cape Town and the pharmacokinetic (PK) and pharmacodynamic (PD) team at LSTM. This talk was given at a TEDx event using the TED conference format but independently organized by a local community.
Experiences of a TB patient
Fatima Karmadwala, TB patient, and student at Liverpool John Moores University talks to Heather Toner, TB Nurse Specialist Lead, Royal Liverpool University Hospital about the hurdles she had to overcome in the process of diagnosis and treatment of TB, which later turned into MDR-TB.
This interview was part of the session: Global and local perspectives on improving access to TB care filmed at the LSTM Future Focus Event, Thursday, 28 November 2019

IMPACT TB, led by LSTM’s Dr. Maxine Caws, is implementing and evaluating alternative case-finding strategies for TB in communities in Nepal and Vietnam. The consortium, which includes Karolinska Institute (Sweden), KNCV (Netherlands), University of Melbourne (Australia) and Johns Hopkins University (USA), FIT Vietnam and Birat Nepal Medical Trust aims to provide evidence to support policy decisions by National Tuberculosis Programmes on practical strategies to achieve the END TB strategy in low and middle-income countries.

LSTM coordinated the recruitment of over 1,250 participants over 6 months at 4 Liverpool NHS sites, and 3 further afield in Wales, Scotland and Leicester. In this observational study, the device collected breath from patients suspected to have bacterial respiratory tract infection. The study aims to identify biomarkers (volatile organic compounds) in exhaled breath to differentiate between a bacterial and non-bacterial infection by collating a large dataset.
TB Diagnostics
The Centre for Drugs and Diagnostics at LSTM work extensively with industry to design and improve TB diagnostics using their extensive culture collection and Containment Level 3 Facilities at LSTM. The Centre can facilitate the limit of detection experiments and can extend to clinical studies with our partners in high-TB endemic regions including Moldova, Nigeria, and Ethiopia.