World NTD Day 2020
#BeatNTDs: For good. For all

Thursday 30 January marks the first World NTD Day
Neglected Tropical Diseases threaten more than 1,5 billion people living in the poorest and most marginalised communities worldwide. LSTM is one of the more than 250 organisations which have signed up to mark this day to raise awareness and mobilise greater attention, action, and investment to ensure progress continues to be made in combatting these debilitating diseases.
LSTM is at the forefront of Neglected Tropical Diseases (NTDs) research and works to identify critical bottlenecks in the field of NTDs through its research and implementation activities, whilst evaluating alternative strategies to overcome the existing barriers and to improve strategies for their control and elimination.
LSTM focuses on a multidisciplinary approach to NTDs building on the particular strengths of its academic departments. This draws together a broad range of existing NTD expertise and creates new areas for collaborative programmes across LSTM.
LSTM’s Centre for Neglected Tropical Diseases (CNTD) continued their key role in the implementation of control and elimination NTD programmes with a new £15m three-year award from DFID’s Accelerating the Control and Elimination of Neglected Tropical Disease (ASCEND) programme targeting five of the worst NTDs: lymphatic filariasis, onchocerciasis, schistosomiasis, visceral leishmaniasis and trachoma in 25 of the world’s poorest countries.
World NTD Day Seminar
On the eve of the first ever World NTD Day, the seminar showcased LSTM’s newly expanded Centre for Neglected Tropical Diseases with speed talks to illustrate the breadth of translational research and impacts of our neglected tropical disease activities.
Mass Drug Administration
CNTD is a major implementing partner of UKAid’s investment into the Global NTD Programme and has delivered the DFID funded LF Elimination Programme since 2009. The Centre provides strategic and technical support to national programmes in its 12 project countries to carry out their NTD programmes and has provided preventive chemotherapy treatments for LF to over 200 million people since 2009.
In 2019 LSTM’s Centre for Neglected Tropical Diseases (CNTD) was awarded £15m as part of DFID’s flagship ASCEND (Accelerating the Control and Elimination of Neglected Tropical Disease) programme in partnership with Sightsavers, The Schistosomiasis Control Initiative and Mott MacDonald.
The funding will support the implementation of mass drug administration and morbidity management and disability prevention for five of the worst NTDs: lymphatic filariasis, onchocerciasis, schistosomiasis, visceral leishmaniasis and trachoma in 25 of the world’s poorest countries. CNTD will cover 13 of these countries in West and Central Africa.

Eliminating Lymphatic Filariasis
CNTD’s programme has treated over 280 million people and trained over 500,000 people to administer the drugs within their communities.
CNTD also focusses on treating those with acute infections, predominantly swollen limbs (lymphoedema) and hydrocele (scrotal swelling). These conditions are often disabling and cause suffering to families as sufferers are frequently unable to work or participate in normal family life.
CNTD, one of the main implementing partners of WHO’s Global Programme to Eliminate Lymphatic Filariasis, continues to provide technical support to national NTD programmes in more than 20 countries across sub-Saharan Africa and Asia.

Developing macrofilaricide candidates for filarial diseases
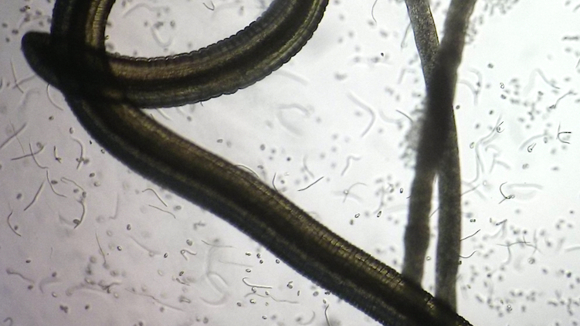
Lymphatic filariasis (elephantiasis) and onchocerciasis (river blindness) are two important neglected tropical diseases that cause severe disability and affect more than 157 million people globally. Control efforts are hindered by the lack of a safe macrofilaricidal (adult parasite killing) drug.
Targeting the Wolbachia bacterial endosymbionts in these parasites with doxycycline leads to a macrofilaricidal outcome but protracted treatment regimens and contraindications restrict its widespread implementation.
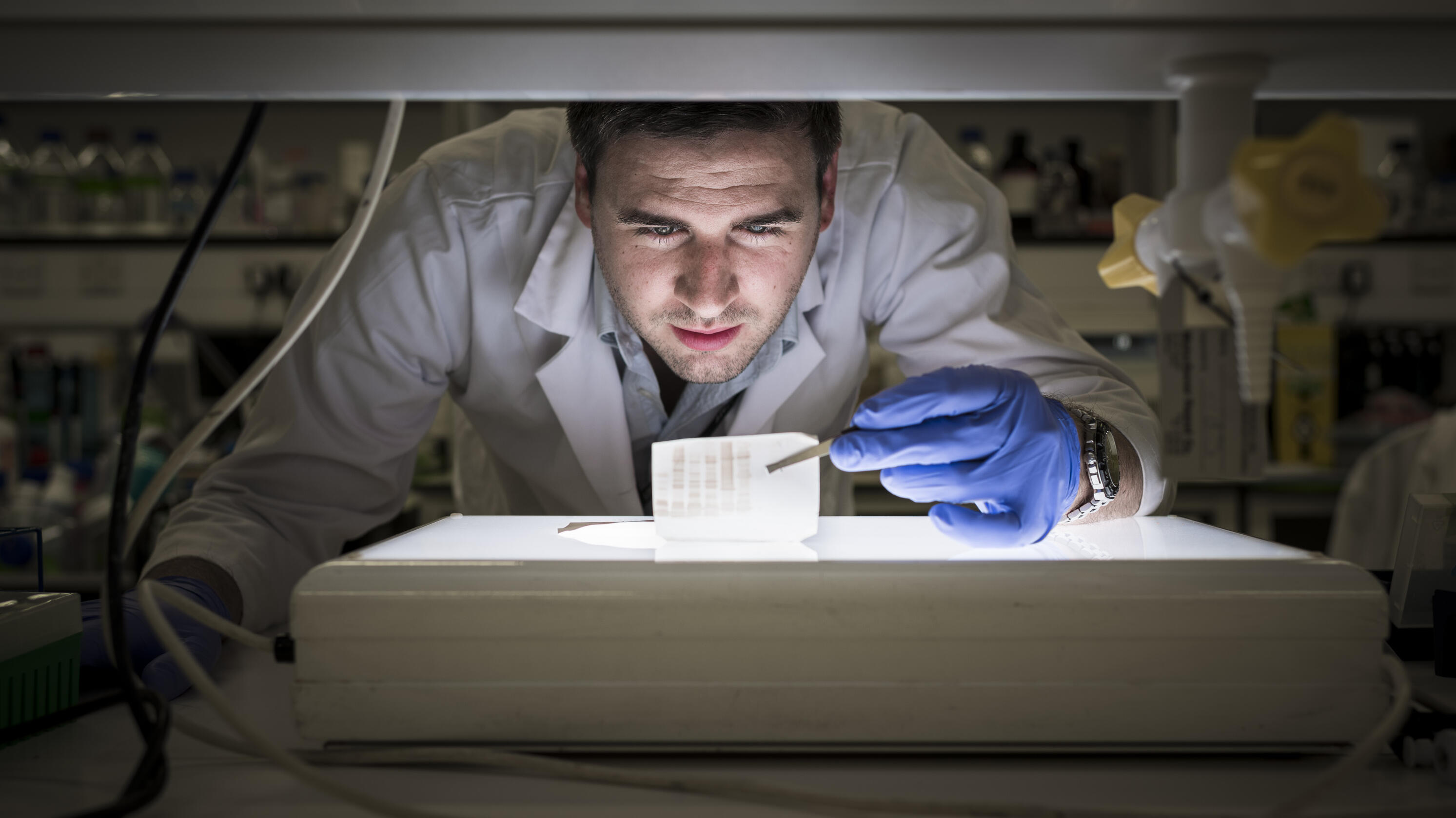
As part of an ongoing macrofilaricide drug discovery project LSTM successfully completed a lead optimisation programme to deliver a pre-clinical candidate anti-Wolbachia based macrofilaricide.
A·WOL, led by Professors Mark Taylor and Steve Ward with Dr Joe Turner, continues to progress new drug candidates for safe macrofilaricidal drugs for onchocerciasis and lymphatic filariasis.
The discovery and development of A·WOL’s first candidate selected anti-wolbachial drug, a re-purposed macrolide ABBV-4083 (TylaMac), was published in Science Translational Medicine and has successfully completed Phase I testing in humans and is now progressing to Phase II testing in DRC in partnership with Abbvie and DNDi.
The highly selective anti-wolbachial drug, AWZ1066 was published in the Proceedings of the National Academy of Science and is undergoing formal pre-clinical development through MRC DPFS funding in partnership with Eisai.
Other publications include our collaboration with AstraZeneca’s High-Throughput Screening Group to screen 1.3m compounds from AZ’s collection in just 10 weeks generating 20,000 hits and 9 chemical series with rapid and potent anti-wolbachial activity as published in Nature Communications.
A·WOL is also working to identify the targets of our new drugs and to understand the mode-of-action of our new rapid-kill compounds with the aim to further reduce the treatment regimens for onchocerciasis and lymphatic filariasis.
Alumni spotlight: Dr. Louis Paluku Sabuni
Dr. Louis Paluku Sabuni is an LSTM graduate and achieved his Ph.D. from LSTM. He is currently the Leprosy Mission’s country leader in DR Congo and affiliated to the Universite Officielle de Rwenzori (Public University of Rwenzori, Butembo, North Kivu/DRC. All TLM’s projects in the country have two underlying goals: that persons affected by leprosy and other neglected tropical diseases should have access to integrated quality service in each district; and that the way TLM works with communities affected by leprosy should result in long-term sustainable improvements in their lives.
A new focus on genital schistosomiasis in women and men

As part of expanded workplans of COUNTDOWN, it has recently drawn attention to female genital schistosomiasis (FGS) in Ghana and for health systems to adapt and respond appropriately.
Using a qualitative method approach, community members and associated health workers were interviewed to find widespread misconceptions about FGS. The signs and symptoms of this disease were confused with other sexually transmitted infections such that adolescent girls who reported with vaginal discharge and itching were often stigmatised by health workers for promiscuity, which left their FGS incorrectly managed.
Looking to the future, integration of praziquantel treatment within sexual and reproductive health services in primary health care services may raise the profile of this unrecognised condition and provide guidelines for its treatment.
Urogenital schistosomiasis is caused by infection with Schistosoma haematobium, an important parasitic disease in sub-Saharan Africa and is well-known to cause significant damage to the urinary tract.
This aspect of disease gives rise to either female genital schistosomiasis (FGS) or male genital schistosomiasis (MGS), where eggs of the parasite damage the internal or external genitalia. To draw international attention on this aspect of disease, several LSTM staff assisted COR-NTD to hold a discussion workshop in Liverpool, to assess its importance with HIV infection, cervical cancers and women’s wellbeing in general.
With regard to MGS, a systematic review of cases reported across the globe has been conducted by PhD student Dr Seke Kayuni, a research clinician from Malawi. Many adult fishermen who are on antiretroviral therapy exhibit classic MGS where eggs of S. haematobium can be found in semen, as well as cause overt damage to tissues. Since all current diagnostics in use for MGS are imperfect, it is important to take an integrated diagnostic approach to better manage MGS patients.
The Centre for Snakebite Research & Interventions (CSRI)
LSTM’s expanding snakebite research portfolio reflects the global situation. Thus, in the past two years, the tropical snakebite disease domain has been radically transformed from a globally neglected medical condition dismissed as an ‘injury or accident’ to a WHO priority Neglected Tropical Disease.
In May 2019, WHO launched its strategy to halve global snakebite mortality and morbidity rates by 2030. LSTM’s Professors Harrison and Lalloo were lead writers of this new strategy to reduce the 138,000 deaths and 400,000 disabilities caused by snakebite every year.
Led by Professor Rob Harrison and with £9.6m funding by the Department for International Development for the Scientific Research Partnership for Neglected Tropical Snakebite (SRPNTS) project, CSRI has added the development of monoclonal antibody-based next-generation snakebite therapies to LSTMs therapy-discovery portfolio.