
Advancing the clinical and public health management of multi-drug resistant tuberculosis (MDR-TB)
Pathways of least resistance
LSTM has advanced the management of multidrug-resistant Tuberculosis management across several areas of pioneering research.
This research has involved simulation modelling helping guide changes to the diagnostic process, changes to treatment regimens (TB-drugs), and the delivery of these drugs to patients.
Tuberculosis and Multidrug-resistant Tuberculosis: An overview

Tuberculosis (TB) is the world’s leading cause of death from an infectious agent. Today about 30,000 people will fall ill with tuberculosis, and 4,000 people will die from the disease. Tuberculosis usually affects the lungs, and is caused by the bacillus Mycobacterium tuberculosis which is spread through the air by coughing and speaking. Multidrug resistant TB (MDR-TB) is caused by an organism that is resistant to at least rifampicin and isoniazid, the two most common drugs used to treat TB. These drug-resistant forms of TB are posing a significant public health crisis, being a major contributor to deaths from antimicrobial resistance globally and affecting approximately half a million people each year.
Costs faced by tuberculosis patients
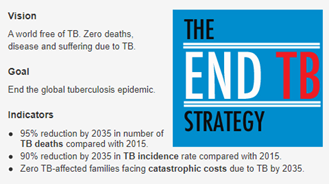
Despite TB testing and TB drugs being free in most high TB-burden countries, TB patients face considerable costs in their journeys to getting diagnosed and throughout their treatment. These costs include charges for things such as health services, transportation, accommodation, and nutritional supplements, as well as lost income due to inability to work. We also know that these costs are higher for patients with multidrug-resistant TB. Recognition of this cost burden led to the setting of policy goals around financial protection of patients and the elimination of catastrophic care-seeking costs in the WHO’s End TB strategy.
A systematic review on financial burden for TB patients conducted by Tanimura and colleagues in low and middle-income countries showed that on average TB patients spend almost $900, with half of these costs before the start of treatment. This was equivalent to 58% of the patients’ reported annual individual income, higher among those patients with MDR-TB.
Improving the treatment for MDR-TB: The STREAM trial

STREAM is the world’s largest recruited, multi-country randomised clinical trial to examine shortened regimens for MDR-TB.
Prior to the STREAM 1 trial, WHO recommended the 9-11-month short regimen based on ‘very low quality’ evidence, so the shorter treatment had to be tested in a randomised trial setting. The health economic component led by LSTM showed that the short-regimen leads to economic benefits for health systems and patients. These benefits are substantial, even when taking into account additional costs of safety monitoring (as high-dose moxifloxacin and clofazimine administered in the short regimen were known to increase the risk of prolongation of the QT interval- a measurement made on an electrocardiogram used to assess some of the electrical properties of the heart, and thus increase the possibility of adverse events).
Squire, Langley, and Rosu participated in dissemination and discussion of the preliminary results of both the clinical and economic elements of the trial, including to the WHO Guideline Group in 2018 . These and the final published results, demonstrating non-inferiority of the 9-11-month regimen (compared to 20 month), contributed to the formulation of two updates to the WHO guidance on management of MDR-TB [3,4] and the WHO 2019 consolidated guidance endorsing shortened regimens with economic benefits for both patients and health systems [5]. The shortened MDR-TB regimen has already benefitted 200,000 people, with 82 countries having adopted it. The beneficiaries are predominantly poor people with TB in low- and middle-income countries (LMIC). Conservatively assuming a resultant health system cost saving of USD1,545 and direct patient cost saving of USD238 per patient (as calculated for Ethiopia), an overall societal cost saving of USD357 million was achieved in 2018.
The methodology developed in the STREAM trial is currently being used in further work:
- Phase 2 of the STREAM trial
- The “Cost and cost-effectiveness analysis” section of the ShORRT operational research package developed by WHO/TDR to support rollout (currently in Benin, DRC, Pakistan and Nigeria) of all-oral shortened, primarily home-based MDR-TB regimens. These all-oral regimens will permit wide-scale shift to out-patient management of MDR-TB resulting in further savings for patients and health systems.

Transitioning to out-patient management of MDR-TB

Financial well-being of MDR-TB patients and their households is a function of duration of treatment, but also driven by the extent to which treatment is delivered through in-patient care. Modelling of the data in STREAM 1 established that an out-patient model would lead to significant health system cost savings compared to an in-patient model. These findings fed into the global discussions (STAG-TB) on the need to shift to all-oral regimens in general to facilitate out-patient care. WHO issued a rapid communication in Dec 2019 recommending this shift but only recommending rollout of the 9 month all-oral regimen under operational research conditions and for certain patients; those without extensive disease and without resistance to fluoroquinolines. LSTM supported implementation of this recommendation through contribution to the ShORRT package which is now being used to rollout all-oral, home-based MDR-TB treatment in several countries, including Nigeria, Pakistan, Benin and DRC.
Malawi moved to primarily home-based, fully oral MDR-TB treatment lasting 18-24 months from March 2020. While injectables are no longer needed for MDR-TB in Malawi, it should be noted that the home-based care trial demonstrated that training patient-nominated lay people to deliver injectables offers a sustainable opportunity for home-based management of patients with forms of drug-resistant tuberculosis, such as extensively resistant TB (XDR-TB), where injectables are still required .
Predictive Simulation Modelling for Rollout of Molecular Diagnosis for MDR-TB

There are multiple ways to diagnose tuberculosis, and each health setting is unique. Decision makers must choose between different testing technologies, and where to place them within health systems. With competing strategies providing different accuracies in their results, varying in their length of time and the demand they place on both health resources and patients, it is critical policy makers are able to predict the effect of rolling out a new strategy when allocating health budgets.
LSTM has pioneered the utilisation of operational models to represent health systems virtually. This approach has been used since 2014 to guide policy-making in the diagnosis of TB and MDR-TB in many countries, including Brazil, Russia, South Africa, Tanzania, Ethiopia, Philippines, Kenya, and Nepal. With the support of our collaborators Lanner, we use Witness predictive simulation software to represent health systems virtually, capturing and reflecting complex patient-pathways. Such modelling allows us to see how inputs such as equipment availability, diagnostic accuracies, patient heterogeneity and process times, affect the performance and costs of a strategy.
In our Tanzania modelling we used an integrated model to assess the effects of different algorithms of GeneXpert and LED fluorescence microscopy in Tanzania. We found that full scale-up of Xpert would have the greatest population-level effect, with the highest cost, though health economic analyses determined that this would be cost-effective.
Philippines TB-FIT Modelling
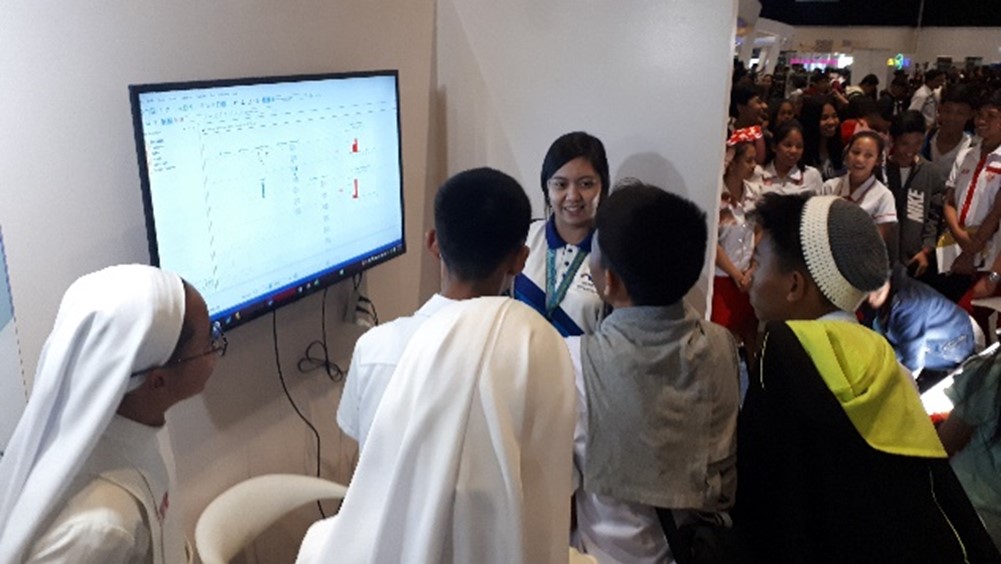
In the TB-FIT project we built a virtual health system model to compare impacts and cost-effectiveness of multiple diagnostic strategies for TB and MDR-TB diagnosis in Cavite Province, Philippines. Strategies were evaluated from a societal and health system perspective. We found that the optimum strategy for diagnostic yield was full rollout of GeneXpert Ultra for most sites, with the primary benefit coming from the additional identification of patients with MDR-TB, with this increase ranging considerably from 22% to 220% between sites.
Professor Charles Yu of Da La Salle Medical And Health Sciences Institute discussing our virtual health system modelling collaboration for the TB-FIT projects in Philippines.
Advocacy and method development

As a member of the Board of The International Union Against Tuberculosis and Lung Disease (2003-2016) including 3 years as President (2008-2011), and a member of the Strategic and Technical Advisory Group for TB (STAG-TB) of the WHO (2016-2018), Professor Squire has played a leading advocacy role for equity-focussed approaches to TB management. He has played a pivotal role in ensuring that the impact on patient costs is incorporated into economic analysis of TB interventions and models of care, contributing to the inclusion of the target to end catastrophic costs for TB patients in the WHO End TB Strategy, launched in 2015. As a member of the WHO Task Force on patient costs, he worked with Ewan Tomeny and international colleagues to develop a robust methodology for assessing TB patient costs . This methodology has become the gold standard for assessing patient costs, and Squire and team incorporated this into within-trial economic evaluations with the latest development being the inclusion of quality of life assessments.
LSTM Seminar: About Time: Advancing the clinical and public health management of drug resistant tuberculosis
This seminar gives an overview of the ways in which LSTM’s collaborative work has contributed to changes in WHO guidelines for the management of MDR-TB.
LSTM's Professor Bertie Squire, Laura Rosu and Ewan Tomeny present highlights of the research, including Operational Modelling of new diagnostics and diagnostic pathways in the Philippines, the health economic evaluation of the multi-centre STREAM Trial, and home-based delivery of injectable medicines in Malawi.
This is followed by a panel discussion on how the research is leading to reductions in time spent by people with TB on health facility attendances for diagnosis, treatment and follow up. These time savings are all contributing to reductions in patient costs and improvements in livelihoods and wellbeing.
The panel participants are:
Prof Sarah Meredith, Professor of Clinical Trials at UCL
Dr Gopalan Narendran, National Institute for Research in TB,
Indian Council of Medical Research Chennai
Dr Charles Yu, De La Salle Health Sciences Institute, Philippines
Dr Corinne Merle, Special Programme for
Research & Training in Tropical Diseases (TDR), WHO
Dr Gillian Turner – Senior Health Adviser,
UK Foreign, Commonwealth & Development Office, Pakistan
#TheClockIsTicking World TB Day 2021
Research Outputs
Langley I,Lin H-H, Egwaga S, Doulla B, Ku C-C, Murray M, Cohen T, Squire SB (2014). Assessment of the patient, health system, and population effects of Xpert MTB/RIF and alternative diagnostics for tuberculosis in Tanzania: an integrated modelling approach. Lancet Global Health, Volume 2, Issue 10, Pages e581 - e591 doi:10.1016/S2214-109X(14)70291-8.
Langley I, Squire SB, Dacombe R, Madan J, E Silva JR, Barreira D, Galliez R, Oliveira MM, Fujiwara PI, Kritski A. (2015) Developments in Impact Assessment of New Diagnostic Algorithms for Tuberculosis Control. Clin Infect Dis. 2015 Oct 15;61Suppl 3:S126-34. doi: 10.1093/cid/civ580
Nunn AJ, Phillips PPJ, Meredith SK, Chiang CY, Conradie F, Dalai D, van Deun A, Dat PT, Lan N, Master I, Mebrahtu T, Meressa D, Moodliar R, Ngubane N, Sanders K, Squire SB, Torrea G, Tsogt B, Rusen ID; STREAM Study Collaborators. (2019) A Trial of a Shorter Regimen for Rifampicin-resistant Tuberculosis. New England Journal of Medicine2019; 380(13):1201-1213 doi10.1056/NEJMoa1811867
Madan JJ, Rosu L, Girma M, van Rensburg C, Evans D, Langley I, Tomeny E, Nunn A, Rusen ID, Squire SB. (2020) STREAM: Economic evaluation of a short-standardised regimen for the treatment of rifampicin-resistant tuberculosis Bulletin of the WHO2020;98:297-372 doi.org/10.2471/BLT.20.000520
Abouyannis M,Dacombe R, Dambe I, Mpunga M, Faragher B, Gausi F, Ndhlovu H, Kachiza C, Suarez P, Mundy C, Banda HT, Nyasulu I, Squire SB (2014). Drug resistance of Mycobacterium tuberculosis in Malawi. Bulletin of the WHO 2014; 92:798-806. doi: 10.2471/BLT.13.126532
Cohen DB, Mbendera K, Maheswaran H, Mukaka M, Mangochi H, Phiri L, Mpunga J, Madan J, Davies G, Corbett E, Squire SB (2019). Delivery of Long-Term Injectable Agents for Tuberculosis by Lay Carers: A Pragmatic Randomised Trial. 2019 Thorax http://dx.doi.org/10.1136/thoraxjnl-2018-212675
The STREAM study is made possible by the United States Agency for International Development (USAID) through the TREAT TB Cooperative Agreement No. GHN-A-00-08-00004, with additional funding for STREAM Stage 1 from the United Kingdom Medical Research Council (MRC) and the United Kingdom Department for International Development (DFID) under the MRC/DFID Concordat agreement. STREAM Stage 2 is being funded by USAID and Janssen Pharmaceuticals, the maker of bedaquiline, with additional support from MRC and DFID.
The contents are the responsibility of LSTM and do not necessarily reflect the views of USAID or the United States Government.”







